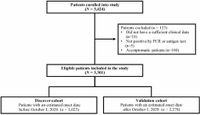
In a significant advancement in predictive medicine, researchers from the Japan COVID-19 Task Force have developed a cutting-edge predictive model aimed at assessing COVID-19 severity using an explainable machine learning approach. The study, published on March 19, 2025, involved a cohort of 3,301 patients diagnosed with COVID-19 between February 2020 and October 2022, shedding new light on how data can guide clinical decisions.
The need for accurate methods to predict the course of COVID-19 has been ever more pressing, as the clinical spectrum of the disease ranges from mild symptoms to critical conditions. Identifying patients at high risk of developing severe disease is crucial, particularly as healthcare systems struggle under pandemic pressures. The model developed by the research team achieved an impressive area under the receiver operating characteristic curve (AUC) score of ≥ 0.905. This was accomplished through the evaluation of just four critical features: serum albumin levels, lactate dehydrogenase (LDH) levels, age, and neutrophil count.
The predictive power of this model was confirmed in two distinct cohorts. In the discovery cohort of 1,023 patients, the predictive model reached a peak AUC of 0.906, with a sensitivity of 0.842 and specificity of 0.811. In validation with a further 2,278 patients, an AUC score of 0.861 was achieved, with a sensitivity of 0.804 and specificity of 0.675.
The research not only highlights the significance of machine learning in current medical practice but also showcases the potential for developing straightforward predictive models that can potentially transform patient management. As stated in the study, "simple and well-structured predictive models were established, which may aid in patient management and the selection of therapeutic interventions." This straightforward approach is essential for broader clinical applicability.
The methodology employed is both innovative and practical. The researchers utilized pointwise linear and logistic regression models within a reinforcement learning framework to accurately evaluate the relationships between various clinical features and severity outcomes. This model construction helped in mitigating common issues faced in machine learning efforts, such as overfitting—where a model performs exceptionally well on training data but poorly on unseen data.
For the study, data were meticulously collected from four different institutions across Japan, ensuring a diverse and representative patient population. The cohort consisted of adults aged 18 and older who tested positive for COVID-19 through PCR or antigen tests. Evaluating both clinical and laboratory data, the study dissected various biomarkers known to influence COVID-19 severity.
Among these biomarkers, age has consistently emerged as a significant predictor of COVID-19 outcomes, with older individuals often facing higher risks of severe illness and mortality. Other factors such as elevated levels of LDH and hypoalbuminemia further compound the risks associated with severe COVID-19. The research took these considerations into account, ultimately distilling the patient data down to essential biomarkers that could effectively guide clinical actions.
This predictive model is particularly remarkable as an early machine learning solution that bridges the gap between complex data and actionable healthcare insights. According to the authors, "This is the first study to establish an explanatory ML-based predictive model for COVID-19 severity that avoids the risk of overfitting and has high reproducibility." This feature ensures that the model's findings can be more reliably applied in real-world settings, presenting an invaluable tool for clinicians managing COVID-19 patients.
Ultimately, the introduction of such models represents a pivotal move towards enhancing patient care and optimizing resource allocation in healthcare systems worldwide. As public health officials and healthcare providers continue to confront the ongoing challenges posed by the COVID-19 pandemic, this research could pave the way for more refined and effective strategies in identifying and intervening in high-risk cases.
The model's successful validation across a multi-center landscape strengthens its reliability and relevance. By targeting high-risk patients with specific interventions based on their predicted outcomes, healthcare providers can offer tailored treatment and support, potentially improving survivorship rates and streamlining care processes.
This promising development is a glimmer of hope in the continuing battle against COVID-19, illustrating how comprehensive data analysis, bolstered by machine learning, can revolutionize the way we predict and treat conditions that significantly impact public health.