In a groundbreaking study published in Nature Communications, researchers have unveiled a novel approach to diagnosing urinary tract infections (UTIs) using metabolomics, a field that analyzes metabolic profiles to identify disease markers. This innovative method could significantly enhance the speed and accuracy of UTI diagnoses.
UTIs are among the most common bacterial infections, affecting millions globally each year and causing over eight million healthcare visits annually in the U.S. alone. The traditional diagnostic workflow for detecting UTIs requires up to 48 hours for urine cultures to identify the bacteria responsible, often resulting in delayed treatment. Current methods rely heavily on the growth of microbes which may yield a negative result even in symptomatic patients, leading to unnecessary antibiotic prescriptions in as many as 70% of cases.
The research team, led by scientists from Alberta Precision Laboratories, set out to develop a metabolomics-based diagnostic tool by investigating the unique metabolites produced by UTI pathogens. Their work focused on analyzing urine samples from patients with suspected UTIs through untargeted metabolomics, which examines various metabolites without predefined targets.
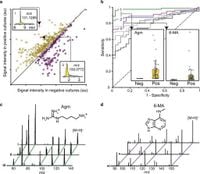
From this analysis, two key metabolites emerged as significant biomarkers: agmatine and N6-methyladenine. Agmatine, a derivative of arginine, and N6-methyladenine, a nucleobase modification, were found to correlate strongly with positive urine cultures. In fact, the presence of these metabolites enables a rapid diagnosis, differentiating between culture-positive and culture-negative samples effectively.
The team developed a streamlined 3.2-minute liquid chromatography-mass spectrometry (LC-MS) assay to quantify these metabolites directly from urine samples. In extensive testing across two blinded cohorts totaling 1,629 patient specimens, the assay demonstrated impressive results: an area under the curve (AUC) of over 0.95 for agmatine and 0.89 for N6-methyladenine, accurately identifying infections caused by 13 Enterobacterales species as well as 3 non-Enterobacterales species. This means that the new method can identify over 90% of UTI-causing pathogens.
Specifically, a diagnostic threshold was established where agmatine concentrations above 174 nM predicted Enterobacterales infections with a sensitivity of 94% and specificity of 97%. Similarly, N6-methyladenine levels accurately distinguished culture-negative urine from non-Enterobacterales UTI specimens, achieving 91% sensitivity and 83% specificity.
Prior studies have suggested potential biomarkers for UTI diagnosis, traditionally focusing on the microbial metabolites associated with E. coli, the most common UTI pathogen. However, this research expands upon that by validating metabolites across a wider range of pathogen species, addressing a critical gap in previous diagnostic approaches that were often limited in scope.
The findings suggest that clinical laboratories could potentially adopt these metabolomics techniques quickly, given that LC-MS equipment is already utilized in many diagnostic settings for other analyses. Thus, while traditional cultures take up to 48 hours for results, this metabolomics approach could enhance diagnostic speeds substantially and reduce the time it takes to initiate appropriate treatment.
Furthermore, this approach offers a dual benefit: not only does it provide faster results but it also holds the promise of reducing the excessive use of antibiotics currently seen in UTI treatment. The new method can help clinicians make informed decisions about antibiotic therapy tailored to the specific pathogens responsible for an infection, potentially curbing the rise of antimicrobial resistance.
Nonetheless, the researchers caution that this metabolomics-based strategy identifies bacteriuria (high levels of bacteria in urine) and must be interpreted alongside clinical symptoms to confirm infection. The single marker model focused on agmatine seems to offer better performance compared to a combined model with N6-methyladenine due to the limited prevalence of the latter in UTIs.
This paradigm shift in diagnosing UTIs points to an exciting future where rapid and accurate metabolic profiling could become a standard in clinical diagnostics, paving the way for improving patient care in urinary infections.
In summary, the integration of metabolomics into UTI diagnostics showcases an innovative step forward, leveraging the complexities of microbial metabolism to transform how we detect and treat infections. The findings of this study could soon inform clinical updates and provide robust evidence for the efficacy of metabolite screening in routine diagnostic workflows.