Scientists at the Wuhan Institute of Virology (WIV) have identified a new coronavirus variant, dubbed HKU5-CoV-2, which can potentially infect human cells via the ACE2 receptor. This receptor was also pivotal during the spread of the COVID-19 pandemic, making the discovery particularly concerning.
Despite no human infections having been recorded from this variant yet, the announcement has triggered significant reactions globally, including increases in shares for vaccine manufacturers, underscoring continuing fears about zoonotic threats—that is, diseases jumping from animals to humans.
Historically, pandemics have shaped human civilization, with past outbreaks like the plague, smallpox, and the Spanish flu leaving lasting impacts. Even with advancements made since those times, new threats continue to emerge at alarming rates. Factors such as deforestation, urbanization, intensive agriculture, and climate change have all been linked to the acceleration of new zoonotic diseases.
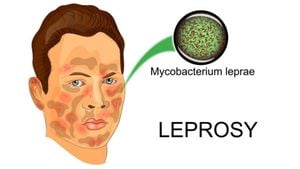
The HKU5-CoV-2 strain was isolated from bats across several provinces, including Guangdong, Fujian, Zhejiang, Anhui, and Guangxi, as part of extensive surveillance efforts. Research led by prominent virologist Shi Zhengli has revealed the variant’s capacity to bind to the ACE2 receptor—just like SARS-CoV-2, which caused the COVID-19 pandemic.
Reports suggest the HKU5-CoV-2 variant may pose serious risks not just to humans but could also infect various mammal species, thereby enhancing the chances of new transmission pathways. "Research on such variants is necessary to understand their potential impact on human health," noted experts, emphasizing the need for continued vigilance.
The global reaction has highlighted persistent uncertainties and fears surrounding zoonotic diseases, with many experts advocating for more stringent monitoring of wildlife and their interactions with humans. Given the rapidly changing dynamics of global travel and commerce, the opportunity for pathogens to spread between species is heightened. This is concerning when considering the increase of international flights pre-pandemic, which reached around 4.5 billion passenger journeys by 2019, and created pathways for diseases to reach new areas.
The underlying conditions leading to the emergence of new pathogens are complex, but researchers have identified several contributing factors. Human encroachment on natural habitats has drastically reduced spaces for wildlife, causing animals and humans to interact more closely than before.
Among these factors include urban expansion, which has led to the rise of new wildlife populations like rats, raccoons, and other animals thriving on human refuse. Intensive livestock farming has also been implicated, as pathogens can jump from wild animals to farmed livestock and humans. Lastly, climate change is forcing some disease vectors like mosquitoes to adapt to new environments, thereby spreading diseases like dengue and Zika.
Mitigative measures implemented during the COVID-19 pandemic—such as improved testing technologies and proactive monitoring of wastewater—are now being evaluated for future use. A global approach is increasingly recommended, integrating public health initiatives within wildlife management to shrink the risk of upcoming pandemics.
Researchers agree the public must remain informed about potential future threats from newly identified viruses like HKU5-CoV-2. The situation emphasizes the need for enhanced collaboration between governments, health organizations, and researchers to develop strong preventative strategies.
With the ever-present threat of disease emergence, learning from past pandemics and incorporating technological advancements is more important than ever as society navigates the complex interplay of health, environment, and global interactions.