The relationship between mean arterial pressure (MAP) and mortality risk has long been studied, but new research sheds light on its complex influence, particularly among patients experiencing acute myocardial infarction (AMI). A recent study from the eICU database has uncovered significant insights, establishing both low and high MAP levels as detrimental to patient survival within the first 28 days of Intensive Care Unit (ICU) admission.
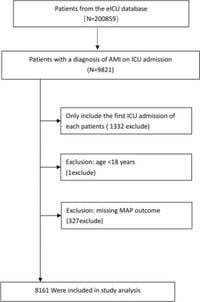
Conducted by researchers analyzing data from 8161 ICU patients, the study reveals alarming statistics: 602 individuals, or approximately 7.38%, succumbed within 28 days of their ICU admission. This analysis aimed to dissect the thresholds of MAP measurements and their correlation to mortality risk, offering fresh perspectives on clinical management strategies.
Significantly, the study identified 84 mmHg as the threshold value for MAP—a point where the relationship with mortality sharply diverges. Below this level, every 10 mmHg increase corresponds to approximately 40.13% mortality reduction, where each 1 mmHg adjustment leads to about 5% drop in mortality rates (OR = 0.95, 95% CI (0.93, 0.96), p < 0.0001). Conversely, when MAP exceeds this threshold, the stakes turn high—each 10 mmHg increase raises the mortality risk by 34.39%. Specifically, each additional 1 mmHg increase beyond the threshold leads to a 3% escalation in mortality risk (OR = 1.03, 95% CI (1.02, 1.03), p < 0.0001).
The underlying implication of this U-shaped curve is stark: within the range of 57 to 110 mmHg, patients exhibit the lowest risk of all-cause mortality. Notably, lower MAP values (40 to 56 mmHg) correlate significantly with increased mortality risks when compared to moderate and higher MAP ranges, illustrating the importance of closely monitoring blood pressure for critically ill patients.
The research builds upon the known significance of MAP as a hemodynamic indicator, which reflects the adequacy of blood flow to organs—particularly relevant during acute situations such as myocardial infarction. Due to the severity associated with AMI, ensuring optimal MAP levels becomes imperative, as either extreme can restrict adequate organ perfusion or cause systemic stress responses.
Many factors were adjusted within the study, including age, gender, race, and comorbidities, ensuring the robustness of these findings. For clinicians, this data is pivotal; it not only reiterates the necessity for vigilant MAP management upon ICU admission but also inspires future investigative endeavors to clarify how these factors interlace and affect mortality risk at varying MAP levels.
Through this retrospective cohort analysis, the complexity tied to MAP and mortality risk has been richly depicted, positioning the study as groundbreaking within the ambit of cardiovascular research. Researchers posited, "This study provides important insights needed for optimizing management strategies for AMI patients and improving clinical outcomes," reinforcing the weight of clinical optimization. The necessity of proactive intervention within the first 12 to 24 hours post-admission cannot be overstated.
Given this study's limitations—particularly concerning unmeasured confounding factors—the authors imply the need for large-scale, prospective studies to solidify these correlations and develop recommendations to guide clinical practice.
Future endeavors should focus on dissecting the exact mechanistic pathways linking MAP levels to health outcomes, such as cardiovascular events leading to mortality, to develop targeted therapies aimed at stabilizing MAP levels among AMI patients. Drawing connections between retrospective findings and clinical practice will be key to enhancing patient care and outcomes within ICU settings.
Overall, the findings underscored the necessity of maintaining MAP within defined ranges, highlighting how both low and high extremes can lead to increased mortality within critically ill patients. With MAP being pivotal for organ perfusion and overall patient prognosis, adhering to comprehensive monitoring can significantly improve outcomes for patients grappling with acute myocardial infarction.