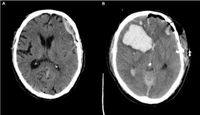
In a comprehensive retrospective analysis, researchers have examined the intricacies of prophylactic anticoagulation in patients suffering from severe traumatic brain injuries (TBI) characterized by acute subdural hematoma (SDH). This investigation primarily focused on the timing of anticoagulant therapies and their influence on postoperative outcomes, particularly the risks of postoperative intracranial hemorrhage (PH) and thromboembolic events (TE).
The study included 259 patients treated between January 1, 2014, and December 31, 2019, revealing critical insights into the impacts of anticoagulation timing. The research is timely, as the demographic aging of populations makes conditions such as atrial fibrillation and the need for anticoagulation increasingly prominent in cases of severe TBI, often resulting from low-impact falls rather than high-velocity trauma.
Notably, the analysis found that prophylactic anticoagulation within 24 to 48 hours after surgery did not correlate with an increased incidence of postoperative hemorrhage. This outcome challenges previous concerns regarding the safety of anticoagulants in such scenarios, suggesting that timely prophylactic anticoagulation does not worsen bleeding risks in these patients.
Among the patients analyzed, 34 experienced PH, with 28 requiring surgical intervention. The study identified that only a small fraction (4 out of 34) of those with postoperative hemorrhage were anticoagulated prior to the event. This data underscores that delayed anticoagulation was more common in patients who ultimately had complications.
Furthermore, the research indicated that patients with PH faced a significantly higher mortality rate within 30 days of surgery, emphasizing the critical nature of managing anticoagulation in this vulnerable population. The results elucidate the risks associated with delayed anticoagulation, establishing a clearer understanding of how timing impacts patient outcomes.
The authors, who conducted the research at Leipzig University, utilized robust statistical analyses to support their findings, including receiver operating characteristic curve analyses and logistic regression. Their careful focus on the correlation between anticoagulation timing and adverse events provides valuable insight into clinical practices that could enhance postoperative care for TBI patients with SDH.
Ultimately, this research highlights the importance of individualized patient care and strategic decision-making regarding anticoagulation therapy in the immediate postoperative period following severe brain injuries. By clarifying the safety of anticoagulant use in TBI patients, the study offers guidance that may influence future clinical protocols.
In light of these findings, it is crucial for healthcare providers to consider the established correlations when managing the therapeutic approach for patients with severe TBI to reduce complications and improve long-term outcomes.