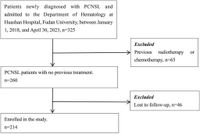
Recent research has shed light on the complex relationship between epilepsy and primary central nervous system lymphoma (PCNSL), a rare but aggressive form of cancer that affects the brain. The study, undertaken by researchers at Huashan Hospital, Fudan University, involved a comprehensive analysis of 214 patients diagnosed with PCNSL between January 2018 and April 2023. Notably, the findings reveal that approximately 16.82% of these patients developed epilepsy, with cortical involvement being a significant risk factor for the onset of seizures.
The prevalence of epilepsy among patients with PCNSL is a crucial aspect of understanding the overall prognosis of individuals battling this disease. Of the 214 patients studied, 36 were identified as having epilepsy, with seizures being the initial symptom in 20 of these cases. This aligns with previous literature that suggests a notable occurrence of seizure activity among brain tumor patients, raising questions about the mechanisms behind this correlation.
One of the surprising results from the research indicated that antiepileptic drugs (AEDs), commonly prescribed to manage seizures, did not significantly reduce the incidence of seizures nor improve progression-free survival (PFS) rates among those with PCNSL. The study reported that AEDs were ineffective in altering the frequency of seizure incidents in the patient population examined, suggesting a need to rethink standard prophylactic treatment practices.
Researchers identified a strong correlation between seizures and cortical involvement in brain lesions. Specifically, patients with cortical lesions exhibited an odds ratio of 9.512 for developing seizures, confirmed by statistical analysis (p = 0.036). Additionally, factors such as an edema zone greater than 1 cm around the lesion and the absence of PIM1 gene mutations may further raise seizure risk.
The findings highlight the importance of determining effective management strategies for patients diagnosed with PCNSL, a condition that currently presents several therapeutic challenges. This unique study not only adds to the growing body of literature on the relationship between seizures and brain tumors but also emphasizes the necessity of tailored treatment protocols to mitigate the impact of both the disease and its complications.
Historically, PCNSL has been a challenging diagnosis due to its aggressive nature and poor prognosis. The standard frontline treatment typically involves high-dose methotrexate (HD-MTX) based chemotherapies, which have been associated with a five-year overall survival rate of approximately 30%. Nevertheless, 15-25% of patients experience resistance to treatment while 25-50% may relapse after an initial response. These factors contribute to the pressing need for ongoing research into better management strategies for patients.
The study revealed that the mean follow-up duration for patients with epilepsy was 1.9 years, during which the incidence of the first seizure was estimated at 89.96 per 1,000 person-years. Among the cohort with epilepsy, 19.44% experienced persistent seizures, while the majority had transient events lasting seconds to hours. Understanding the patterns of seizure occurrence can help inform treatment and ultimately improve quality of life for PCNSL patients.
Interestingly, the study's results challenge the common practice of prescribing AEDs as a preventive measure for patients who have not yet experienced seizures. Instead of reducing the incidence of seizures, the data demonstrated that prophylactic administration of these medications may not be warranted. This poses significant implications for clinical practice in the management of seizures in PCNSL patients.
Furthermore, the research points to the growing need for comprehensive assessments of molecular factors that may influence seizure occurrence in this patient population. With the identification of potential genetic risk factors related to PIM1 mutation status and the role of cortical lesions, the findings underline the complexity of PCNSL and its interactions with neurological comorbidities.
Ultimately, a multidisciplinary approach, including collaboration among neurologists, oncologists, and other healthcare professionals, will be essential in improving patient outcomes in PCNSL, particularly concerning seizure management. The study provides a solid foundation for future research that could inform targeted prophylactic strategies and elucidate the factors contributing to epilepsy in PCNSL patients.
In conclusion, the findings of this extensive study indicate that seizures are prevalent among patients with PCNSL, particularly in those with cortical lesions. However, the ineffectiveness of AEDs in preventing seizures raises important questions regarding treatment protocols and underscores the necessity for tailored management strategies. Ongoing research is needed to evaluate the role of specific genetic mutations and further understand the complexities of how epilepsy interacts with PCNSL.