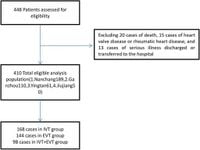
A multicenter retrospective study has provided new insights into the management of anticoagulation therapy for patients suffering from acute ischemic stroke (AIS) due to non-valvular atrial fibrillation (NVAF). Conducted across four tertiary hospitals in Jiangxi Province, the study analyzed clinical data from 410 patients who underwent reperfusion treatments such as intravenous thrombolysis (IVT) or endovascular thrombectomy (EVT) between January 2019 and January 2022.
The researchers found that only 42.7% of patients initiated anticoagulation therapy within the recommended time frame of 14 days following the stroke. Specifically, those in the IVT group were more likely to start anticoagulation sooner than those in the EVT or combined IVT + EVT groups (49.7% vs. 30.3% and 20.0%, respectively). This significant difference underscores ongoing challenges in meeting clinical guidelines designed to optimize stroke recovery.
According to the authors of the article, "the initiation of anticoagulation therapy within the recommended time window is essential to prevent secondary ischemic strokes and improve overall patient outcomes." Their analysis points to prior use of antiplatelet drugs as a common factor among individuals who began anticoagulation early, revealing an odds ratio (OR) of 0.122 that demonstrates a significant correlation.
The findings are crucial because patients who did not receive anticoagulation had worse outcomes, evidenced by higher National Institutes of Health Stroke Scale (NIHSS) scores—indicating greater neurologic impairment—three days after reperfusion (OR = 1.109). Furthermore, these patients experienced a higher rate of in-hospital hemorrhagic transformation, reinforcing the importance of timely anticoagulant initiation.
By the 90-day evaluation period, a total of 281 of the 410 patients achieved a favorable prognosis, as determined by a modified Rankin Score (mRS) of 0-2. This group included an impressive 86.9% of those who received early anticoagulation, compared to only 54.9% among those with delayed treatment—highlighting the stark contrast in outcomes directly linked to the timing of therapy initiation.
Despite the clear clinical benefits associated with early anticoagulation, many patients continued to receive treatment significantly later than guidelines suggest, often due to factors such as large infarct sizes, the specific locations of strokes, and post-stroke hemorrhagic transformations. In fact, physician surveys revealed that approximately 40.83% of decisions related to anticoagulation initiation were influenced by these clinical considerations.
The research further confirms the validity of accelerated treatment protocols. An analysis of recurrent ischemic strokes during the 90-day follow-up showed only 25 cases (6.1% overall), though this did not reach statistical significance when comparing groups. Likewise, vulnerability to complications from bleeding was similar across the board, with 27 bleeding events (6.6%) reported at the same interval.
Overall, while the results emphasize the efficacy of early anticoagulation for AIS patients with NVAF, they also starkly reveal that adherence to timing recommendations remains deficient in real-world clinical settings. The authors state that "most patients received anticoagulation much later than currently recommended," urging for a more streamlined approach in clinical practice to enhance outcomes for at-risk stroke patients and align with established protocols.
As the study progresses, it will be crucial for clinical teams managing stroke cases to focus on reducing barriers to timely anticoagulation. This reflection on treatment delays signifies an opportunity for healthcare systems to reevaluate their protocols and training on stroke management, especially in the context of maintaining optimal patient care amidst the complexities of acute interventions.