In Japan, a recent retrospective cohort study evaluated RhD-negative pregnancies and their management, contributing vital insights into the health approach in obstetrics. This study, conducted across 47 facilities from April 2018 to March 2023, found that RhD-negative instances among pregnant women were notably low and management practices were critical to prevent hemolytic disease of the fetus and newborn (HDFN).
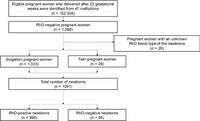
The study identified a mere 0.71% of the total cohort, comprising 152,526 eligible women, were RhD-negative pregnant women. Specifically, 1,088 RhD-negative women participated, and 1,062 met the analysis criteria. Out of these pregnancies, 8.7% of newborns were also RhD-negative. Maintaining proper management of RhD-negative pregnancies is crucial, as exposure to RhD-positive fetal blood can lead to maternal sensitization and the production of harmful anti-D antibodies.
The findings from this research revealed that anti-D immunoglobulin—a standard treatment administered to pregnant women to prevent sensitization—was given to 96.5% of RhD-negative pregnancies. Notably, maternal spontaneous sensitization was assessed, revealing a 0.6% rate before 28 weeks of gestation, with no sensitization detected following this point.
As expected, sensitized women faced more significant risks related to cesarean sections, preterm deliveries, and neonatal complications. Particularly, the instance of neonatal hemolytic anemia was markedly higher among newborns from sensitized mothers, necessitating further medical intervention, such as neonatal intensive care unit (NICU) admissions. These barriers signify the importance of regular testing and monitoring for RhD-negative pregnant women.
During the study period, an indirect Coombs test—a procedure to determine the presence of anti-D antibodies—was performed on 90.7% of the subjects in their first trimester. Follow-ups showed different positivity rates: 4.7% at approximately 28 weeks of gestation and 17.3% postpartum, highlighting ongoing monitoring's relevance.
Researchers indicated that furthering the use of non-invasive prenatal diagnosis of fetal RhD status could significantly improve care efficiency. By using maternal blood and advanced genetic testing methods, medical professionals could avoid unnecessary exposures to anti-D immunoglobulin and optimize healthcare resources.
Dr. Takahashi, one of the study's authors, asserted, "Despite the low incidence of RhD-negative pregnancies, this study underscores the need for tailored management strategies." Current strategies may not align with the unique genetic circumstances found within Japanese genetic backgrounds compared to Western populations, where obstetric practices differ widely.
Compared to other ethnic groups in the world, RhD-negative individuals are significantly less common among East Asians, implicating different healthcare demand dynamics. The study highlights that while the overall management of RhD-negative pregnancies appears effective, the unique situation of the Japanese population warrants consideration to rectify any potential oversight in clinical protocols.
Despite compliance and implementation of guidelines mostly being favorable, certain inaccuracies were observed. For example, in 3.5% of cases, women who should have been treated with anti-D immunoglobulin did not receive the necessary dosage. Such mismanagement can lead to additional risks for both mothers and their infants.
Looking forward, the research lays out a clear argument for adopting advanced techniques in identifying fetal RhD status more widely in Japan. The ultimate goal is to bypass unnecessary anti-D immunoglobulin administrations and preemptively address the risks of sensitization, which can culminate in notable perinatal complications if left unchecked.
As the need for high-quality maternal care evolves, the study points to an imperative for ongoing investigation into integrating innovative prenatal diagnostics into routine care, aligning with best global practices to enhance maternal and neonatal health outcomes in Japan.
In conclusion, the study calls for a careful evaluation of how resource utilization, technology, and management can be better adapted to improve outcomes for RhD-negative pregnancies in Japan. Further research is necessary to cement the study's recommendations and ensure that every pregnant woman receives the optimal care she deserves.