Colorectal cancer remains one of the leading causes of cancer death worldwide, emphasizing the urgent need for advancements in its prognostication and treatment. A recent study has highlighted the promising role of self-supervised learning (SSL) techniques for extracting histopathological features from whole slide images (WSIs) of colon adenocarcinoma, aiming to improve personalized treatment approaches. This innovative research, utilizing data from The Cancer Genome Atlas (TCGA) and the Bevacizumab-Avastin® adjuVANT (AVANT) trial, identifies and characterizes 47 distinct histomorphological phenotype clusters (HPCs), each linked to patients' survival outcomes.
Traditionally, diagnosing colon cancer required pathologists to analyze H&E-stained slides, relying heavily on annotated data and extensive patient histories. The complexity of contemporary healthcare, coupled with increasing patient numbers and advanced biomarker research, makes this process time-consuming and prone to variability. To counter these challenges, researchers have turned to deep learning algorithms to streamline diagnosis, yet these systems still face issues of interpretability and data reliance on human annotations.
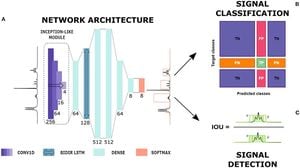
The researchers employed the Barlow Twins model, an SSL framework, to extract relevant features from unannotated WSIs of colon adenocarcinoma, systematically reducing the need for extensive manual input. They analyzed 435 WSIs from the TCGA and constructed 47 distinct HPCs using Leiden community detection algorithms. Each HPC is characterized based on tissue types, architecture, and the immune microenvironment, providing valuable insights on the interplay between histopathology and patient outcomes.
"We shine light on the factors influencing survival and responses to treatments of standard adjuvant chemotherapy and experimental therapies," wrote the authors. This approach has yielded not only clinically relevant insights but also facilitated the mapping of tumor characteristics such as immune composition, stroma variations, and histopathological patterns.
The clinical applicability of the research was validated using data from the AVANT trial, comprising 1213 patients with diagnostic WSIs. The HPC-based classifier demonstrated independent prognostic significance, achieving c-index scores of 0.65 for predicting overall survival, which significantly outperformed conventional prediction models based on clinical variables like age and tumor-stroma ratios.
While the innovative approach demonstrates strong potential for prognostication, the authors caution about limitations inherent to the study. "The identification of HPCs was based on small image tiles...while information about the larger contexts is likely lost," they noted. This recognition of potential pitfalls underlines the need for continuous refinement of prediction models and methodologies.
Importantly, the research draws attention to the complex tumor microenvironment's influence on survival outcomes. The characteristics of the HPCs, for example, show notable correlations with immune infiltrates and oncogenic pathways—elements increasingly recognized as significant players affecting treatment responses. These results reaffirm the advancing intersection of AI with oncology.
Moving forward, the integration of the HPC-based analysis within regular pathology reports could revolutionize how colorectal cancer treatment strategies are determined. The groundwork is laid for developing AI-supported systems to predict responses to various therapeutic approaches, facilitated by the HPC compositions. The research demonstrates how data-driven, machine learning techniques can augment human expertise, fostering optimal, personalized patient care.
For oncologists and pathologists alike, the insights derived from the study could markedly improve the current methods of risk stratification and treatment planning. By continuing to leverage large datasets and advanced machine learning capabilities, the potential exists not only for more accurate predictions but also for improved patient outcomes across diverse treatment regimens.
With the promise of SSL models showcased here, future research will likely focus on refining these techniques, broadening applications, and validating findings across diverse patient populations and treatment scenarios. The ultimate goal remains to integrate these advanced algorithms seamlessly within clinical workflows, empowering clinicians to provide personalized, evidence-based care to patients battling colon cancer.