Chronic skin ulcers pose significant challenges for affected individuals, often leading to severe health complications when left untreated. A new study utilizing Two-Sample Mendelian Randomization (TSMR) has uncovered potential causal relationships between plasma metabolites and chronic skin ulcer risks, providing valuable insights for early prevention and intervention.
The research analyzed data from two substantial cohorts comprising 14,296 participants with 913 metabolites from INTERVAL/EPIC-Norfolk and 8,299 participants with 1,091 metabolites from the Canadian Longitudinal Study on Aging. Outcome data was sourced from finngen_R9_L12_CHRONICULCEROFSKIN, encompassing 1,840 cases versus 353,088 controls, and the UK Biobank Chronic ulcer of skin dataset, which included 495 cases among 455,853 controls.
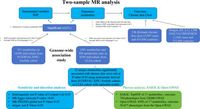
By leveraging advanced statistical methods, including the Inverse-Variance Weighted (IVW) method, along with MR-Egger and MR-PRESSO for sensitivity analysis, the study identified 12 distinct metabolites significantly associated with chronic skin ulcers. An important finding was that the metabolite X-19,141 showed the highest reproducibility regarding its association with chronic skin ulcer risk.
The findings of this study are particularly significant as chronic skin ulcers, often related to underlying conditions like diabetes and vascular diseases, challenge both clinicians and patients. Notably, the intricate pathophysiology leading to these ulcers involves compromised local circulation and aberrant immune responses, which the study aims to address through metabolic markers.
Historically, the research has struggled to prioritize early detection of chronic skin ulcers. While treatments for existing ulcers have improved in recent years—thanks to advancements such as innovative wound dressings and immunotherapy—there remains a critical gap regarding initial identification and proactive measures. This research focuses on addressing this gap and emphasizes the need for early detection strategies engrained with personalized approaches based on individual metabolite levels.
Through the TSMR approach, this study espoused several objectives, including the identification of causal metabolites and deriving early predictive markers for proactive diagnostics. With these tools, clinicians can effectively strategize interventions targeting the metabolic precursors of chronic skin ulcers.
The rigorous methodology for this TSMR analysis consisted of selecting genetic variants strongly associated with plasma metabolites, ensuring adherence to defined statistical criteria to minimize biases inherent to observational studies. The identification process stemmed from robust genomic-wide association studies (GWAS) from two distinct cohorts, which provided instrumental variables for evaluating metabolite associations.
In its extensive analysis across the cohorts, distinct causal links were established, reinforcing the significance of metabolites such as X-19141 and erythronate. These revelations illustrate that specific metabolite profiles are potentially predictive of the risk of developing chronic skin ulcers, hinting at valuable implications for therapeutic targets.
With the exploration of phenome-wide Mendelian randomization (Phe-MR) analysis, researchers delved into relationships between identified metabolites with other diseases or health characteristics. Notably, X-19,141 levels displayed notable correlations with five diseases such as iron metabolism disorders and gout, broadening its clinical relevance as a biomarker.
These findings not only enhance our understanding of the mechanisms underlying chronic skin ulcers but offer a roadmap for tailoring individualized approaches to treatment and prevention strategies targeting specific metabolites. Viewed through this lens, the metabolites identified could engender a paradigm shift toward personalized medical care in managing chronic skin ulcers.
However, the study acknowledges limitations, particularly disparities in instrumental variables that may arise from cohort differences and sample size variances. Future studies should address these constraints, further validating the metabolic pathways linked to chronic skin ulcers.
The authors advocate for the possible integration of these metabolites into routine clinical assessments to improve early diagnosis, thereby enabling timely interventions that could prevent the transition to chronic ulcers. With X-19,141 emerging as a pivotal metabolite marker, the hope lies in leveraging its consistent associations to refine risk stratification methodologies that can augment current clinical practices.
In conclusion, this study paves the way for innovative strategies that could enhance patient outcomes and limit the burden of chronic skin ulcers. Such forward-thinking research is essential as we continue to unravel the complexities of chronic skin ulcer pathology and the role metabolic interventions can play in patient care.