In a study involving 353 hospitalized children with Mycoplasma pneumoniae pneumonia, researchers found that co-infections with other pathogens are common and could complicate treatment and recovery. More than 40% of the children with Mycoplasma pneumoniae, a viral infection prevalent in pediatric patients, were found to have additional respiratory infections.
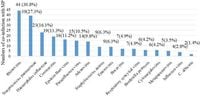
The study, conducted at the Women and Children’s Hospital of Ganzhou between May 2023 and July 2024, reveals that acute Mycoplasma pneumoniae pneumonia can often coexist with various viral and bacterial infections, raising concerns about treatment efficacy and the risk of severe illness. The most common co-infecting pathogen identified was Rhinovirus in 30.8% of the cases, followed by Streptococcus pneumoniae (27.3%) and Haemophilus influenzae (16.1%).
Understanding how these additional infections interact with Mycoplasma pneumoniae pneumonia is crucial for proper management. Among those with co-infections, 57.3% had just one additional pathogen, while some children had up to five. Notably, those in the co-infection group faced a greater likelihood of developing severe pneumonia and showed higher rates of resistance to macrolide antibiotics.
Previous research has shown that Mycoplasma pneumoniae pneumonia can account for over 40% of pediatric community-acquired pneumonia cases during epidemic years, yet studies on the impact of these co-infections have been limited. This analysis aims to fill that knowledge gap as respiratory illnesses ramp up during colder months.
The methodology involved a retrospective analysis of collected data, which included bright and clear identification of Mycoplasma pneumoniae through various testing protocols, including bronchoalveolar lavage (BAL), where doctors cleared respiratory fluid to examine it for pathogens. The findings of this study provide eye-opening data, as 40.5% had co-infections characterized by significant challenges in treatment due to a higher risk of drug resistance and severe health complications.
Among the outcomes observed, significant differences were identified between the groups with single Mycoplasma pneumoniae infections and those with co-infections. A higher incidence of severe pneumonia was noted in the co-infected children, with statistical significance evident across various measures.
The study's conclusions indicate that clinicians should be cautious about diagnosing and treating Mycoplasma pneumoniae pneumonia, especially in cases where co-infection is suspected. The interaction between pathogens can complicate the clinical picture, leading to increased hospitalization days and greater healthcare costs.
Furthermore, the increase in macrolide resistance rates emphasizes the need for vigilant monitoring and possibly revisiting treatment protocols in pediatric patients. As researchers continue to explore these intricacies, their findings are set to influence future practices for managing pneumonia in children, particularly during peak infection seasons, which have significant public health implications.