A recent study has found a positive correlation between triglyceride glucose-body mass index (TyG-BMI) and hypertension (HTN) among American adults, highlighting the potential of this innovative measurement as a simple tool for early detection of high blood pressure risks.
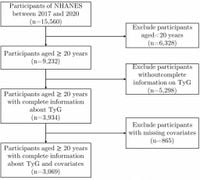
The research, published on March 17, 2025, examined data from the National Health and Nutrition Examination Survey (NHANES) database, focusing on 3,069 adults aged 20 and older. The study's principal investigator, Lin Zhao, along with their team, aimed to determine if TyG-BMI could serve as a cost-effective surrogate marker for insulin resistance, which has been linked to the incidence of hypertension.
Hypertension, affecting nearly 30% of adults globally, has significant health and economic impacts, leading to various complications such as heart disease and stroke. Despite its prevalence, evaluating the risk factors for hypertension typically relies on more complex and costly methods, such as the high insulin-normal glucose clamp. This complexity has led to the search for simpler indices like TyG-BMI to assess insulin resistance.
TyG-BMI combines measurements of triglycerides, fasting blood glucose, and body mass index, making it accessible and easier to calculate. The study found, "For every 10-unit increase in the TyG-BMI, the risk of HTN increases by 4.3% (95% CI: 1.00701.08, P = 0.018)," highlighting its significant association with hypertension prevalence.
Age, as revealed by stratified analyses, plays a notable role; the correlation between TyG-BMI and hypertension is particularly strong among individuals aged 60 years or older (P < 0.05). This result aligns with the larger trend of increased hypertension risk with advancing age, warranting targeted preventive measures for older demographics.
To establish the relationship between TyG-BMI and hypertension, the research employed multivariate logistic regression models. These analyses confirmed the strength of the association across various demographic factors, establishing TyG-BMI as potentially pivotal to monitoring health risks associated with hypertension.
The study's results also pointed to a nonlinear relationship between TyG-BMI and hypertension; as TyG-BMI values increased past 242.192, the accompanying rise in hypertension risk became statistically insignificant. This finding emphasizes the need for careful monitoring of TyG-BMI, particularly for those exceeding the inflection point.
Hypertension disproportionately affects different racial groups, and this study accounted for demographic factors, ensuring the robustness of its conclusions across the diverse U.S. population. The positive correlation it established reinforces the need for large-scale, cost-effective screening methods for hypertension using accessible markers like TyG-BMI.
Overall, the findings advocate for routine monitoring of TyG-BMI as part of preventative health strategies, potentially reducing the healthcare burden associated with hypertension. Researchers recommend increasing awareness among healthcare providers to utilize TyG-BMI measurements as part of routine assessment, particularly for older adults who demonstrate higher susceptibility.
With hypertension on the rise, the introduction of easily calculable indices like TyG-BMI could serve as proactive means to guard against future health crises related to high blood pressure and its associated complications.
While this study provides significant insights, the authors also noted the limitations inherent to cross-sectional studies, which cannot establish causation. They urge the need for longitudinal research to explore the temporal relationship between TyG-BMI and hypertension to confirm its predictive value.
Through efforts to establish clear links between TyG-BMI and increased health risks, this research offers promise not only for hypertension prevention but potentially for higher quality of life and longevity for countless adults as they age.