A recent study has identified the triglyceride/high-density lipoprotein cholesterol (TG/HDL-C) index as a reliable predictor of cardiovascular disease (CVD) risk among individuals with type 2 diabetes mellitus (T2DM), particularly those with retinopathy and hyperlipidemia but no prior history of CVD. The research was part of the EMPATHY trial, which evaluated the effects of intensive versus standard statin therapy on cardiovascular outcomes.
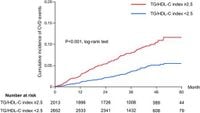
With cardiovascular disease being the leading cause of mortality among T2DM patients, accurate means for assessing risk factors have become increasingly important. The study involved 4,665 participants divided based on their TG/HDL-C index levels—a ratio derived by dividing triglyceride levels by high-density lipoprotein cholesterol levels. Participants classified as high-risk (TG/HDL-C ≥ 2.5) numbered 2,013 compared to 2,652 deemed low-risk (TG/HDL-C < 2.5).
Over the median follow-up period of 36.8 months, the findings illustrated concerning disparities between these groups. Specifically, those within the high TG/HDL-C index threshold experienced significantly higher rates of cardiovascular events, with hazard ratios indicating nearly double the risk of CVD as compared to those with lower values (HR 1.89, 95% CI 1.45–2.47, p < 0.001).
This association raised pivotal questions about the necessary treatment interventions for those classified under the high TG/HDL-C index. Investigation results revealed notable interactions between the TG/HDL-C index and statin treatment allocation, particularly observing how intensive statin therapy appeared to yield reductions in CVD risk for individuals falling under the high-risk category but offered no such benefits for their lower-risk counterparts.
According to the authors of the study, 7TG/HDL-C index ≥ 2.5 was associated with higher CVD risk among T2DM patients with retinopathy and hyperlipidemia without known CVD.7 This insight may lead to susceptibility differentiation, aiming to identify individuals who may benefit from more aggressive therapeutic strategies.
Statistical models employed throughout the study showed consistent associations between the TG/HDL-C index and various cardiovascular events, reaffirming its potential role as a predictive metric within insurance and rehabilitation contexts. The EMPATHY study had previously highlighted the limited effectiveness of standard statin therapy compared to intensive regimens, prompting the need for appropriate stratification of treatment based on heightened cardiovascular risk indices.
The study participants exhibited various characteristics associated with cardiovascular risk, including higher rates of male sex, blood pressure, and smoking, which were more prevalent among those with the elevated TG/HDL-C index. Total CVD events comprised coronary events, cerebrovascular incidents, as well as renal and vascular conditions, significantly affecting the health and operational capabilities of those diagnosed with T2DM.
This thorough analysis serves to underline the urgency of effectively managing rising indications of CVD within diabetes-enduring cohorts, confirming the TG/HDL-C index as it emerges as not just another statistical measure, but rather as key biomarker capable of influencing clinical decision-making.
While the findings propagate significant implications for preventive medicine and clinical practice, the authors caution against preconceived notions surrounding dyslipidemia assessments. They indicate the pivotal role of the TG/HDL-C index should extend beyond just lipid monitoring to incorporate thorough investigations targeting insulin resistance and associated metabolic disorders as well.
Overall, this research may implicate changes to the accepted paradigms of CVD risk assessments for T2DM patients, emphasizing the need to anticipate and mitigate future cardiovascular complications by employing effective patient monitoring protocols and targeted therapies. For patients fitting these outlined demographics, healthcare professionals should re-evaluate lipid management strategies, ensuring they reflect the risk identified through TG/HDL-C evaluations and prioritize empowered self-management education aimed at addressing lifestyle choices contributing to vascular health.
These findings contribute to the growing body of knowledge confirming the urgent necessity of proactive measures for managing diabetes-related complications, underscoring the value of the TG/HDL-C index as both reference and guide.