A recent study published in Scientific Reports reveals critical insights into the intersection of nutrition, inflammation, and mortality among U.S. adults diagnosed with cardiometabolic syndrome (CMS). Using extensive data collected from the National Health and Nutrition Examination Survey (NHANES) between 1999 and 2010, the study underscores the importance of the Advanced Lung Cancer Inflammation Index (ALI) as a powerful predictive tool for assessing mortality risks in this vulnerable population.
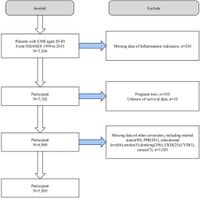
The research indicates that individuals with poor nutritional status and high levels of inflammation experience significantly higher rates of all-cause and cardiovascular mortality. Out of 5,969 study participants, consisting of 2,900 men and 3,069 women, the data revealed 1,753 all-cause deaths and 607 deaths specifically from cardiovascular conditions, highlighting the severe implications of CMS on health outcomes.
Cardiometabolic syndrome itself, characterized by a clustering of metabolic abnormalities such as obesity and insulin resistance, has seen its prevalence rise alarmingly in the United States—from 28.23% in 1999 to 37.09% in 2018. This escalating trend is concerning as it poses substantial risks for cardiovascular diseases and premature death among affected individuals.
Utilizing Kaplan-Meier analysis, the study demonstrated a clear association between enhanced nutrition and reduced inflammation with improved long-term survival rates. The ALI was specifically noted to correlate negatively with mortality outcomes, suggesting that maintaining a favorable ALI could substantially mitigate death rates in patients suffering from CMS.
Further analysis employing COX regression models confirmed that for each unit increase in ALI, the risk of all-cause mortality decreased by 0.4%, and the cardiovascular mortality risk fell by 0.8%. This revelation emphasizes the necessity of encouraging lifestyle modifications that improve nutritional status, given that the appropriate management of inflammation can lead to significant health benefits.
Moreover, the study identified an interesting U-shaped relationship between ALI and all-cause mortality, indicating that while lower ALI levels are linked to greater mortality risk, there exists a critical inflection point at approximately 106.24. Below this threshold, improvements in ALI correlate with lower mortality rates. However, once this point is exceeded, the risk of mortality begins to counterintuitively increase, potentially due to the negative consequences stemming from over-nutrition.
This finding adds another layer of complexity to the understanding of the obesity paradox, where some individuals classified as obese may exhibit lower mortality risk under specific conditions. The study argues for a nuanced interpretation of such outcomes, reminding clinicians of the delicate balance between nutritional excess and deficiency.
Subgroup analyses further explored the applicability of these findings, revealing that different demographic and health factors, such as age and existing health conditions like heart disease or kidney disease, could influence the effectiveness of ALI as a predictor of long-term mortality. Notably, ALI was established as particularly effective for those over 60 years of age and for patients with prior health issues.
The implications of these findings are pressing for healthcare providers. As CMS continues to confront the healthcare system with rising challenges, integrating routine evaluations of ALI could enhance risk stratification and intervention strategies for patients. By fostering optimal nutritional and inflammatory status, healthcare practitioners can significantly influence patient outcomes, extending survival in this significant risk group.
In conclusion, the study argues that maintaining an appropriate ALI level is crucial for mitigating the risk of all-cause and cardiovascular mortality in individuals with CMS. Ensuring access to nutritional resources and implementing effective anti-inflammatory strategies may provide promising pathways for improving patient health outcomes.