A recent study has made significant strides in understanding the relationship between blood flow in the choroid and the complications seen in central serous chorioretinopathy (CSC), particularly focusing on pigment epithelial detachment (PED) and subretinal fluid (SRF). Conducted by a team at the Eastern Renmin Hospital of Wuhan University, the study highlights how changes in choroidal circulation may contribute to visual impairments associated with CSC.
Central serous chorioretinopathy is a condition characterized by serous detachment of the retinal pigment epithelium, leading to symptoms like blurred vision and distortion. While earlier research has pointed towards choroidal thickening as a feature of the disease, this latest study goes further by examining the dynamics of choroidal blood flow and its correlation with various ocular parameters in patients.
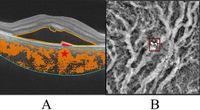
The researchers categorized 53 patients with CSC into two distinct groups: those with PED and those without. They also included an age-matched control group of healthy participants. Utilizing swept-source optical coherence tomography (SS-OCT), they measured several parameters, including the three-dimensional choroidal vascular index (CVI), choroidal vascular volume (CVV), subfoveal choroidal thickness (SFCT), and areas and volumes of SRF and PED. Image analysis was conducted to assess the flow void area (FVa) and flow void area percentage (FV%) within the choriocapillary layers.
Results indicated that patients with CSC showed significantly higher levels of SFCT, CVI, CVV, FVa, and FV% when compared to healthy individuals. Notably, patients with PED had an even greater three-dimensional CVI than those without, with significant statistical support (P < 0.05). Among the CSC cohort, FV% exhibited a positive correlation with SRF area, CVV, and SFCT. Additionally, within the PED subgroup, CVV was positively linked to PED-ct, FVa, FV%, and both PED and SRF area, indicating a complex interplay between blood flow and disease manifestations.
This multifaceted approach is crucial, as traditional assessments using only two-dimensional CVI do not accurately represent the entirety of choroidal vascular changes. The researchers advocate for the three-dimensional CVI as a superior metric for understanding choriocapillary conditions in CSC patients.
As for the implications of these findings, they suggest that the structural changes in choroidal blood vessels may directly affect retinal functionality. The study correlates increased vascular density and lumen expansion in Sattler and Haller layers with fluid accumulation beneath the retinal epithelial layer, further elucidating the pathogenesis of CSC. This chain of events can result in visual distortions and other complications faced by CSC patients.
This research also raises the possibility that monitoring these choroidal parameters could serve as a valuable tool in predicting the progression of CSC-related conditions. The findings could pave the way for enhanced diagnostic criteria and tailored treatment options aimed at alleviating visual impairments.
Although the study offers impressive insights, the authors emphasize certain limitations, such as the need for a larger sample size and longitudinal follow-ups to better assess the clinical implications of observed choroidal changes. Future research should focus on confirming these findings and further exploring the connections between choroidal vascularity and retinal disease progression.
In conclusion, the intricate relationship between choroidal blood flow, PED, and SRF in patients with CSC reveals vital information about the mechanisms driving this condition. Enhanced understanding of these processes could lead to novel therapeutic strategies aimed at improving patient outcomes.