Rheumatoid arthritis (RA), a chronic inflammatory disorder, persists as a major healthcare challenge, demonstrating profound impacts on patients’ quality of life. In light of this, researchers are investigating promising therapies that could better manage the disease, particularly the use of Janus kinase (JAK) inhibitors.
A groundbreaking study published on March 21, 2025, examines the effects of five approved JAK inhibitors on inflammation related to RA, specifically focusing on their capabilities to inhibit interleukin (IL)-6-induced inflammatory and angiogenic factors in human synovial tissues. The research team, based at Kobe University Graduate School of Medicine, set out to address the increasing need for effective therapeutic interventions in patients suffering from this debilitating condition.
IL-6 and tumor necrosis factor alpha (TNFα) are pivotal pro-inflammatory cytokines that play a significant role in the pathogenesis of RA, promoting synovial tissue proliferation and contributing to joint destruction. The aberrant activation of angiogenesis—a process that promotes the growth of new blood vessels—is one of the key aspects of RA progression, necessitating innovative treatment options.
In this study, the researchers compared the effects of five JAK inhibitors: tofacitinib (TOF), baricitinib (BAR), peficitinib (PEF), upadacitinib (UPA), and filgotinib (FIL). These inhibitors target the JAK/STAT pathway, inhibiting the phosphorylation of signal transducer and activator of transcription (STAT) proteins, which are crucial for transmitting signals from cytokines. All five inhibitors demonstrated significant efficacy in suppressing IL-6-induced inflammatory factors, including vascular endothelial growth factor (VEGF) and intercellular adhesion molecule-1 (ICAM1).
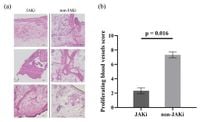
The researchers obtained synovial tissues from six RA patients undergoing total knee joint replacement surgery. These tissues were then subjected to histological analyses and various laboratory techniques to evaluate the efficacy of the JAK inhibitors on inflammatory responses. In their findings, they revealed that the JAK inhibitors led to a marked decrease in angiogenesis, evidenced by diminished lymphocyte infiltration and lower expression of VEGF and ICAM1 in the JAK inhibitor group compared to a control group.
At the heart of the study lies a critical conclusion: "All five JAK inhibitors were effective in reducing IL-6-induced inflammatory and angiogenic factors," as stated by the authors of the article. However, the study also suggested that the specific molecular mechanisms and pharmacological properties of these inhibitors might lead to differing efficacies. For instance, while BAR showed a strong inhibitory effect on ICAM1 and VEGF mRNA expression, TOF did not suppress all inflammatory and angiogenic markers to the same extent as BAR when stimulated with IL-6.
Moreover, the study highlighted the complexity of the JAK/STAT pathway, noting that while all five inhibitors effectively suppressed IL-6-induced inflammation, their effectiveness varied. The inhibitory effects on key inflammatory pathways emphasize the necessity for tailored therapeutic approaches that consider individual patient responses to treatment.
The researchers employed quantitative reverse transcriptase-polymerase chain reaction (RT-PCR) and Western blot analyses to determine the levels of STAT1 and STAT3 protein phosphorylation, both implicated in the inflammatory response. Results showed that all JAK inhibitors significantly reduced pSTAT1 and pSTAT3 levels compared to untreated controls, reinforcing their therapeutic potential.
While this study advances the understanding of JAK inhibitors and their role in RA treatment, it also reveals limitations, such as the small sample size and the lack of long-term data on the safety and effectiveness of these treatments in diverse patient populations. Future studies are warranted to delve deeper into the therapeutic implications of these findings.
In conclusion, this study illuminates the efficacy of JAK inhibitors in inhibiting IL-6-induced inflammation and angiogenesis in RA synovial tissues, positioning them as a critical therapeutic target. As the search for effective RA treatments continues, understanding the nuanced differences among these JAK inhibitors can guide clinicians in maximizing patient outcomes and advancing knowledge in RA management.