Researchers have developed a pioneering prognostic model that highlights the role of methionine metabolism in hepatocellular carcinoma (HCC), a prevalent form of liver cancer. By investigating the enzyme betaine-homocysteine S-methyltransferase (BHMT), they uncovered significant connections between its expression levels and patient outcomes.
The study, conducted on a cohort of 96 HCC patients at Nanchang Ninth Hospital, reveals a crucial link between methionine metabolism and tumor progression. The global incidence of HCC has surged, making it the sixth most diagnosed cancer worldwide. Approximately 80% of primary liver cancer cases are attributed to this disease, causing significant mortality rates. The need for more accurate prognostic models to guide treatment decisions is paramount.
A critical aspect of the research highlights the dependence of HCC cells on methionine, illustrated by the Hoffman effect, which suggests that these cancer cells cannot synthesize methionine effectively, making them reliant on external sources. BHMT, an enzyme implicated in the metabolism of methionine, was found to have diminished expression in HCC tissues, indicating a potential prognostic biomarker.
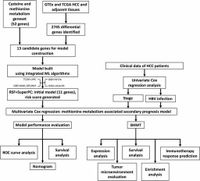
The team employed advanced bioinformatics techniques, analyzing data from various established cancer databases. They constructed and validated a prognostic model that demonstrates considerable predictive power regarding patient outcomes. Notably, lower levels of BHMT expression correlated with poorer overall survival rates.
This novel research underscores the importance of the tumor microenvironment and its metabolic characteristics in relation to HCC progression. The study also revealed that BHMT influences the infiltration of immune cells, particularly M1 macrophages, indicating its possible role in enhancing immune responses against tumors.
Furthermore, the researchers examined how BHMT's expression might serve as a predictive marker for the efficiency of immunotherapy treatments aimed at HCC patients. Samples from a cohort undergoing anti-PD1 immunotherapy demonstrated that patients with high BHMT expression had better therapeutic outcomes, underscoring BHMT's potential as a significant biomarker.
The findings of this research have potential implications for developing new treatment strategies for hepatocellular carcinoma, as they point to the possibility of metabolic interventions in cancer therapy. By leveraging the interactions between tumor metabolism and immunotherapy outcomes, this work opens new avenues for research into personalized medicine approaches for HCC patients.
In summary, the groundbreaking insights into the methionine metabolism-related prognostic model highlight the multifaceted role of BHMT in HCC, paving the way for improved risk stratification and therapeutic decision-making. Future clinical application of these findings could enhance treatment outcomes for patients battling this aggressive cancer.