A new prediction model developed for microvascular obstruction (MVO) occurrence in patients with acute myocardial infarction (AMI) undergoing percutaneous coronary intervention (PCI) holds promise for improved patient management and outcomes. This study, conducted by researchers at the Affiliated Hospital of Xuzhou Medical University, used preoperative clinical data to predict MVO, a condition frequently associated with adverse patient prognoses following AMI.
Ischemic heart disease (IHD), responsible for approximately 12.7% of global deaths, is a significant concern for health worldwide. Acute myocardial infarction, a severe form of IHD, presents critical challenges, especially in managing complications that arise post-reperfusion. MVO occurs in about 40-50% of AMI cases, reflecting the failure of the microvascular system following mechanical reperfusion. Remarkably, it is an independent predictor of adverse cardiovascular events, thereby making early identification crucial.
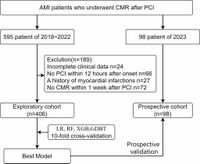
The study's authors sought to develop a multifactor prediction model for MVO risk, leveraging data from patients diagnosed with AMI and who underwent PCI. Over a timeline that spans from January 2018 to August 2023, the researchers included 504 AMI patients in their analysis, segregating them into exploratory and prospective cohorts to validate the model's efficacy.
The model utilized random forest recursive feature elimination (RF-RFE) to identify critical predictors among 29 clinical features collected, such as high-sensitivity troponin T (hs-TnT), neutrophil count, creatine kinase-MB (CK-MB), fibrinogen, and left ventricular ejection fraction (LVEF). Among the various models tested, the logistic regression approach demonstrated the highest predictive performance, achieving an Area Under the Curve (AUC) score of 0.800 in the exploratory cohort and 0.792 in the prospective cohort. This indicates strong reliability in predicting MVO occurrence, which could significantly improve management strategies for AMI patients experiencing PCI.
The prospective validation cohort also revealed that out of the participants, 55 individuals, or 56.1%, were identified with MVO, comparable to the exploratory cohort where 213 (52.5%) had the same condition. Interestingly, this model has been integrated into a user-friendly online platform, allowing healthcare professionals to input preoperative medical information and receive an immediate risk assessment for MVO. This mobile-optimized platform ensures that critical MVO detection can aid in effective decision-making and management strategies.
Additionally, the predictive model's success highlights the vital role of data analytics and machine learning in enhancing patient outcomes in cardiovascular care. By focusing on significant predictors and employing a straightforward model like logistic regression, this method outperformed more complex machine learning approaches. The careful selection of features through the RF-RFE method improved model reliability, facilitating practical application in clinical settings.
Another significant takeaway from this study lies in the understanding of the predictors identified—hs-TnT and CK-MB act as crucial biomarkers for myocardial injury. They demonstrated improved predictive potential when analyzed collectively, showcasing a more nuanced understanding of MVO formation pathways. Neutrophils’ role in inflammation and thrombosis underlines the cellular mechanisms contributing to MVO, and the importance of LVEF in assessing systolic function links directly to left ventricular performance outcomes following an AMI.
Furthermore, the study presents a promising avenue for integrating predictive analytics into routine clinical practice. As highlighted, early identification of high-risk MVO patients could enable personalized management strategies and optimize treatment outcomes in AMI cases.
Despite its promising results, the study acknowledges limitations concerning sample size and its reliance on a single-center cohort—with implications for the broader applicability of its findings. Future research will need to validate and optimize the model through multicenter data collection, ultimately refining its clinical application.
In conclusion, this innovative prediction model for MVO using preoperative clinical data might significantly enhance the personalized management of AMI patients undergoing PCI. The integration of cardiovascular digital medicine into routine practice stands to transform patient prognostic frameworks moving forward.
For health professionals interested in employing this model, it can be accessed through the online platform established by the researchers at the Affiliated Hospital of Xuzhou Medical University at https://mvo.model.smilemed.cn. With the potential to streamline care and improve patient outcomes, this development reflects a step forward in cardiovascular risk management.