Cancer patients who develop acute pulmonary embolism (APE) and require admission to intensive care units (ICUs) face alarming mortality risks within the first 30 days of their treatment. A recent study published on March 18, 2025, has unveiled a new nomogram—a predictive model designed to better estimate short-term mortality in this vulnerable population by examining critical clinical indicators.
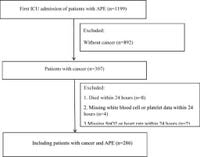
The nomogram arose from a retrospective analysis of data sourced from the MIMIC-IV database, a vast repository of patient information from the Beth Israel Deaconess Medical Center that spans admissions from 2008 to 2019. This study focused on 286 cancer patients diagnosed with APE, with an average age of 68.9 years, revealing a striking 30-day mortality rate of 32.2% among them.
Traditionally, the simplified pulmonary embolism severity index (sPESI) has been employed to predict outcomes in patients with APE. However, its limitations among critically ill cancer patients prompted researchers to explore alternatives. The study sought to validate the sPESI score while simultaneously developing a more effective predictive model tailored specifically for ICU patients.
In analyzing their findings, researchers identified several independent predictors of mortality. Key factors included the Sequential Organ Failure Assessment (SOFA) score, the presence of tumor metastasis, hemoglobin levels, anion gap, patient weight, and the prevalence of liver disease. The research indicates that each of these variables plays a significant role in forecasting the likelihood of a patient’s early death.
The high stakes of acute pulmonary embolism in cancer patients can be attributed to multiple factors, including the disease itself and the associated treatments that predispose patients to develop venous thromboembolism. The connection between cancer and APE is not merely statistical; it underscores the urgent need for accurate prognostic tools to enable proper management and intervention strategies in high-risk patients.
In conducting their retrospective analysis, the authors utilized multivariable logistic regression to assess the relationship between clinical predictors and 30-day mortality rates. Results showed a marked distinction between the predictive values of the established sPESI score and the newly developed nomogram: the area under the curve (AUC) for the sPESI was 0.568 compared to the nomogram's robust AUC of 0.761, indicating the latter's enhanced reliability in anticipating mortality risk.
This new nomogram provides clinicians not only with a statistical tool but also with a clinical advantage in patient management. By utilizing specific inputs pertaining to each patient’s clinical condition, healthcare providers can make informed decisions regarding treatment pathways and identify those who may benefit from closer monitoring and targeted interventions.
Furthermore, findings reveal that tumor metastasis emerges as a particularly weighty predictor, demonstrated through a striking odds ratio of 2.85, signifying that advanced spread of cancer significantly increases the likelihood of early mortality in affected individuals. Moreover, anemia remains a formidable challenge for many cancer patients, with the study noting that lower hemoglobin levels correlate with heightened mortality risks.
Significantly, an elevated anion gap—an indicator of metabolic disturbances—also played a role in risk stratification, showcasing the multifaceted nature of factors influencing mortality outcomes in this cohort. The integration of these indicators into the nomogram suggests a multifactorial approach that could aid clinical teams in addressing the complexities associated with managing cancer patients who present with APE.
As the study illustrates the necessity of refined predictive models tailored to the unique challenges of treating cancer patients, it also calls attention to the importance of future research in this area. While the nomogram represents a step forward, conducting larger, multi-center studies will be essential for further validating these findings and enhancing the predictive capabilities of this tool.
By improving how clinicians assess the risk of mortality in patients battling both cancer and acute pulmonary embolism, we can ensure that more personalized and responsive care is delivered. The ultimate goal remains to enhance the quality of treatment and improve outcomes in a population that is at inherent risk of complex health challenges.
In conclusion, the findings from this research underscore the pressing need for continued advancement in predictive tools for high-risk patients, emphasizing how the integration of clinical parameters into a single, user-friendly model can streamline care in critical settings. As healthcare continues to evolve, the development and application of such tools serve as a cornerstone in the fight against mortality in patients facing acute pulmonary embolism amid cancer diagnosis.