A new predictive model developed by researchers from Guangdong Second Provincial General Hospital is changing the way healthcare professionals assess the risk of recurrent strokes for patients with minor ischemic strokes (MIS). Known as the PLANS model, this innovative tool aims to refine and individualize secondary prevention strategies for these at-risk patients.
With approximately 1 million new cases of ischemic stroke diagnosed annually in China, minor ischemic strokes account for about half of these occurrences. Despite their seemingly less severe nature, MIS patients are at significant risk for recurrent strokes, with 14.7% experiencing repeat cerebrovascular events within one year of their initial incident. The necessity for accurate risk prediction tools is ever-growing, as healthcare providers seek effective methods to administer prevention strategies.
Until now, existing models—such as the Essen Stroke Risk Score—have demonstrated limitations, particularly when assessing patients with MIS. Unlike typical ischemic stroke patients, MIS patients often display milder symptoms, leading to complications not fully captured by traditional assessments. Recognizing this gap, the researchers sought to develop the PLANS model, which incorporates key clinical and lifestyle variables to provide clearer predictions.
The four major components of the PLANS model include physical activity, the presence of large artery strokes, the National Institutes of Health Stroke Scale (NIHSS) score upon admission, and smoking status. Each of these factors carries distinct risk levels. For example, patients exhibiting lower physical activity levels had significantly increased risks of recurrent strokes, with hazard ratios indicating up to three times higher risk compared to those who are actively engaged.
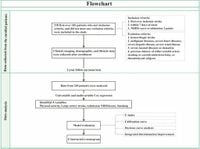
Data collected from 218 patients enrolled between November 2012 and January 2014 indicated the robustness of the PLANS model. Those with large artery strokes experienced much higher risks, aligning with previous findings on the prevalence of this stroke type. With the C-index of 0.780 for the PLANS model exceeding the Essen model’s score of 0.556, the new model offers superior predictive capability, especially important for developing targeted treatments for high-risk individuals.
The study revealed other lifestyle factors influencing stroke recurrence, emphasizing the role of smoking cessation and physical activity adoption. Regular exercise was shown to significantly mitigate risks, underscoring the importance of lifestyle interventions as part of post-stroke care.
"The PLANS model, incorporating both traditional and novel risk factors, provides a valuable tool for patient stratification and personalized secondary prevention strategies," wrote the authors of the article. Their study highlights not just the importance of personalized medical care, but also ways to implement such strategies effectively across diverse patient populations.
One standout feature of the PLANS development is the creation of publicly accessible online nomograms, allowing both healthcare professionals and patients to calculate individual risk probabilities easily. These nomograms are readily available at https://ody-wong.shinyapps.io/PLANS/, highlighting the collaborative effort to improve patient care through innovation and engagement.
Despite its promising findings, the authors acknowledge the need for external validation of the model across various cohorts to confirm its reliability. "External validation in diverse cohorts is warranted to confirm these promising results," they stress, urging future studies to explore comprehensive assessments beyond just stroke risk factors.
The healthcare impact of accurate stroke recurrence predictions cannot be overstated, especially as guidelines suggest intensified preventative measures for high-risk individuals. By enhancing the tools available for healthcare providers, the PLANS model paves the way for significantly improved treatment plans, potentially reducing the rate of recurrent strokes among MIS patients. With continuous refinement and validation, the future of secondary stroke prevention could be bright, fostering greater health outcomes and quality of life for patients.