Obesity is not just a matter of lifestyle; it is deeply embedded in our genetics. A recent extensive meta-analysis has shed light on significant genetic variations linked to body mass index (BMI) across diverse populations, offering new insights into how we understand obesity.
Recognizing the global uptick in obesity rates, which poses a considerable public health challenge, researchers have long sought to decode the underlying genetic factors. The most recent findings explain a considerable portion of why some individuals are more predisposed to obesity, highlighting the interaction between genetic predispositions and environmental triggers.
The study analyzed data from 2,005,180 individuals, which included individuals of European, Asian, and African descent. Through this expansive genome-wide association study (GWAS), researchers pinpointed a significant intergenic deletion at the MC4R locus, highlighting its direct correlation with a 4.11 kg/m2 increase in BMI per allele. This critical deletion potentially contributes to obesity by downregulating the function of the MC4R gene, which is known for its role in the leptin-melanocortin pathway that regulates appetite and body weight.
Furthermore, a rare variant discovered in the FRS3 gene, specifically the missense variant p.Glu115Lys, was found to correlate with a lower BMI, showcasing a potential protective effect against obesity. This variant, primarily identified in Finnish populations, could provide a new avenue for developing obesity treatments targeting specific genetic pathways.
"We identify an intergenic 262,760 base pair deletion at the MC4R locus that associates with 4.11 kg/m2 higher BMI per allele, likely through downregulation of MC4R," stated the authors of the article. As this genetic variant plays a significant role in appetite regulation, its understanding may lead to innovative approaches in treating obesity.
The involvement of FRS3 is especially intriguing as it encodes an adaptor protein tied to critical neurotrophic signaling pathways, implicating it as a crucial player in energy expenditure and appetite regulation. As reported in the study, "Moreover, a rare FRS3 missense variant, p.Glu115Lys, only found in individuals from Finland, associates with 1.09 kg/m2 lower BMI per allele," emphasizing its potential for therapeutic interventions.
Historically, obesity research has faced challenges, particularly concerning the limited representation of diverse populations within genetic studies. This latest research makes strides in addressing these gaps, demonstrating the importance of including varying ancestries to reveal a comprehensive understanding of obesity's genetic architecture. Prior studies often overlooked the significant genetic variations that may exist across different ethnic backgrounds, thereby limiting the applicability of their findings.
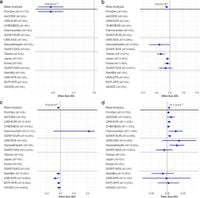
The methodology incorporated in this meta-analysis involved robust statistical techniques to ascertain the association between genetic variants and BMI effectively. Researchers tested nearly 190 million sequence variants, employing stringent significance thresholds to ensure reliable results. Their findings not only corroborate previously identified genetic factors but also introduce new potential targets that could influence obesity risk and treatment strategies.
Examining the implications of these findings, researchers note the crucial role that the MC4R and FRS3 genetic variants may play in therapeutic drug development. The potential to activate the BDNF-TrkB signaling cascade, which is historically linked to appetite control, opens doors for innovative pharmacological approaches targeting these pathways.
Despite the exciting progress made in this area, much remains to be explored. The readouts indicate the need for functional studies to delineate the precise mechanisms through which these identified variants influence BMI and appetite. Additionally, the role of environmental factors and their interplay with genetic predispositions invites further research.
In conclusion, as obesity continues to represent a multifaceted health crisis affecting millions globally, understanding its genetic underpinnings is more critical than ever. This work provides a stepping stone toward identifying new therapeutic mechanisms using genetic insights. By aligning future research with these groundbreaking findings, scientists may uncover tailored strategies that effectively combat obesity, paving the way for improved interventions in public health.