A new computer-assisted method shows promise as a prognostic factor for hepatocellular carcinoma (HCC), following findings that a significant reduction in binuclear hepatocytes in paracancerous tissues may predict short-term recurrence after surgery. The study analyzed 73 patients, with a focus on the abundance of binuclear hepatocytes (ABH), paving the way for more personalized treatment approaches.
Hepatocellular carcinoma (HCC) is a leading cause of cancer-related mortality worldwide, with dismal outcomes typically associated with surgery. The feasibility of adjuvant therapy following surgery is hampered by a lack of effective patient stratification criteria. Current recurrence rates post-surgery remain high, with approximately 20% of patients experiencing tumor relapse within two years. This recurrence is often linked to genetic alterations and the dynamics of the tumor microenvironment, which can serve as a supportive ‘soil’ for tumor ‘seeds.’
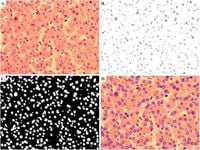
This recent study, published by researchers at Ruijin Hospital, Shanghai, evaluates the potential of ABH as a biomarker for early recurrence. By employing an ImageJ script to analyze histological samples, the study highlighted that HCC patients exhibited a substantially lower ABH compared to those with other liver diseases or benign conditions. Specifically, the findings indicated that HCC patients had an ABH of approximately 4.35%, significantly less than that in benign liver diseases (11.49%) and other liver malignancies (6.79%).
Immunohistochemistry assays conducted within the study supported additional findings suggesting a link between ABH and arginase 1 (ARG1) expression levels, a protein involved in the urea cycle that has been associated with tumor development. The correlation suggests that low levels of ABH may imply compromised liver function and contribute to a worse prognosis in patients with HCC.
The results indicate that patients with decreased ABH were more likely to experience short-term recurrence within two years of surgery, as evidenced by statistical comparisons revealing average ABH levels of just 3.31% in patients who relapsed versus 5.43% in those who did not. Furthermore, ABH was shown to negatively correlate with clinical conditions such as liver cirrhosis and variable ARG1 expression levels. The findings point to ABH’s utility in identifying high-risk patients who may benefit from more intensive monitoring or adjuvant therapy.
Through logistic regression analysis, the study established that both computer-generated values of ABH (cABH) and pathologists’ counted values (pABH) were significant independent predictors for short-term recurrence in HCC patients. This provides clinical validation for employing ABH in patient selection, enhancing the care management of individuals undergoing radical surgery for HCC.
As HCC continues to pose significant treatment challenges, integrating new prognostic indicators such as ABH into clinical protocols could ultimately lead to improved patient outcomes. The research marks a critical step toward refining the selection process for adjuvant therapies, potentially minimizing unnecessary relapses in this high-stakes patient group.
Overall, this study underscores a pivotal intersection of computational analysis and clinical pathology, suggesting that enhanced monitoring of binuclear hepatocytes may become integral in the fight against HCC recurrence.