Nephtrology fellows in Southwest China exhibited a commendable understanding of vascular access for chronic hemodialysis patients, yet they demonstrated moderate attitudes and practices, highlighting the need for enhanced training in specific areas.
Chronic kidney disease (CKD) represents a significant global health challenge, affecting roughly 10% of the global population and 10.8% of the Chinese population, with a striking prevalence of 18.3% in Southwest China alone. Among those diagnosed with end-stage renal disease (ESRD), a leading method of renal replacement therapy (RRT) is hemodialysis, which accounts for 80-90% of cases worldwide. Effective vascular access before commencing hemodialysis is crucial for patient safety and the success of treatment.
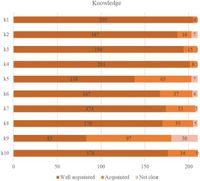
A recent study involving nephrology fellows aimed to quantify their knowledge, attitudes, and practices (KAP) regarding vascular access training. This cross-sectional survey was conducted between June 1 and June 10, 2024, with 210 valid responses collected. Demographically, 54.3% of the fellows were female, and 37.6% were aged between 36 and 40 years. The study revealed that the median score of fellows' knowledge on vascular access was 19 out of a potential 20, indicating a high level of understanding. However, attitudes and practices yielded median scores of 36 out of 50 and 46 out of 80, respectively.
The authors of the article indicated a positive correlation between knowledge and attitudes (Pearson’s r = 0.439, P < 0.001), knowledge and practices (r = 0.645, P < 0.001), and attitudes and practices (r = 0.560, P < 0.001). Mediation analysis established that knowledge and attitudes substantially influenced practical performance, with a direct connection demonstrated through various sociodemographic and experiential factors.
Vascular access is intrinsic to the hemodialysis process; the need for skilled practitioners in this area is paramount. Educational systems presently pose challenges for nephrology fellows, as nearly 56.7% had prior experience leading vascular access-related surgical procedures. The complexity surrounding vascular access establishment highlights the necessity for further training curricula aimed at addressing knowledge gaps, especially concerning monitoring access patency and contemporary guidelines specific to nephrology practice.
The study concluded that nephrology fellows are well-informed regarding vascular access but exhibit moderate attitudes and practices warranting targeted educational strategies to improve outcomes. The findings emphasize enhancing the understanding of recent advances and established protocols surrounding vascular access techniques.
In conclusion, this investigation illuminates crucial avenues for improvement in nephrology fellow training in Southwest China, thereby potentially enhancing patient care standards across the region.