Acute febrile illness (AFI) is a frequent health challenge in Uganda, where a significant portion of such cases remains undiagnosed due to insufficient diagnostic tools. A recent study conducted by researchers from the Uganda Virus Research Institute (UVRI) and the Centers for Disease Control (CDC) sheds light on the viral pathogens responsible for these illnesses, drawing from data collected between 2011 and 2013.
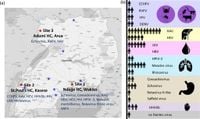
The research examined 1,281 febrile patients from various parts of Uganda, revealing a critical need for improved diagnostic surveillance. Among the participants, who had a median age of 18, 56% were female. The study included samples from central, western, and northern Uganda, emphasizing the geographical diversity of AFI.
Using metagenomic next-generation sequencing (mNGS), researchers discovered viral pathogens in 44 out of 230 undiagnosed samples, which accounts for 19% of cases analyzed. Notably, the study detected high-consequence viruses, including Crimean-Congo hemorrhagic fever (CCHFV), Rift Valley fever (RVFV), dengue (DENV), and yellow fever, in seven patients (3%). An exceptional find was the Le Dantec virus, a pathogen not reported since 1969, suggesting its re-emergence.
One patient infected with CCHFV, a 30-year-old male from Kasese district, presented with fever, headache, and joint pain, lacking awareness of prior tick exposure. He was misdiagnosed and treated with vitamins, but ultimately made afull recovery. This misdiagnosis underscores the risks associated with the limited clinical recognition of viral hemorrhagic fever (VHF) conditions.
Among the 44 patients identified with viral infections, the breakdown included 7 associated with VHF (CCHFV, RVFV, YFV, DENV), 10 linked to respiratory infections, 17 with hepatitis viruses A, B, and E, and 6 with gastroenteritis-causing viruses. Six patients were also found to have infections of human immunodeficiency virus-1 (HIV-1).
The findings highlight a pressing public health concern, as many patients were treated with antibiotics or anti-malarials, which may be inappropriate for viral infections and could contribute to antimicrobial resistance. Additionally, the detection of vaccine-preventable diseases such as hepatitis A and measles among children illustrates the necessity of improved vaccination coverage in Uganda.
Analysis of risk factors associated with viral infection indicated significant correlations with exposure to standing water, which was linked to nearly double the odds of viral infection in the cohort. Furthermore, wall spraying was identified as a protective factor. These findings stress the importance of vector control measures in reducing disease transmission risk.
This study exemplifies the implications of using advanced metagenomic techniques for viral surveillance, particularly in resource-limited settings. The results advocate for enhanced diagnostics and public health strategies in combatting the ongoing burden of febrile illnesses and viral infections in Uganda.
The overall high detection rate of respiratory and gastrointestinal viruses also signals a call for future studies to include non-invasive sample types, such as nasopharyngeal swabs and stool samples, to provide a comprehensive view of viral disease burden. Improved diagnostic approaches could reduce misdiagnoses and optimize patient care across Uganda.
Furthermore, the study highlights the critical role of genomic surveillance in mapping outbreaks and potential emerging threats, advocating for greater investment in public health infrastructure to respond to viral diseases proactively.