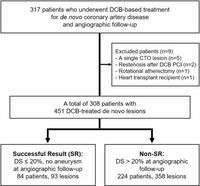
Drug-coated balloons (DCBs) provide a promising therapeutic strategy for treating de novo coronary artery disease (CAD), a common condition where coronary arteries become narrowed due to atherosclerosis. Recent research conducted at Korea University Ansan Hospital illustrates that successful procedural optimization may enhance the efficacy of DCB treatment. A study involving 317 patients undergoing DCB-based interventional procedures revealed significant insights into how various factors can impact treatment outcomes.
The analysis categorized patients into two primary groups—those achieving a successful, stent-like outcome (designated as "SR" with a diameter stenosis of less than 20%) and those not achieving this outcome (termed "Non-SR"). Notably, SR lesions exhibited larger diameters and a greater use of specialty balloons compared to Non-SR lesions, revealing a direct emphasis on the procedural techniques employed. According to the study, reaching a maximal post-DCB minimal luminal diameter (MLD) and a larger balloon-to-artery (B-A) ratio are independent predictors of successful angiographic outcomes.
The study showcased that in the successful SR group, procedural characteristics such as a larger balloon diameter and a higher B-A ratio contributed to achieving an MLD that significantly improved patient outcomes. Specifically, the post-DCB MLD was observed at key thresholds, which were 1.95 mm for MLD and 1.13 for B-A ratio, to positively influence angiographic success.
Notably, at a median follow-up period of eight months, SR lesions also demonstrated lower late lumen loss and indications of favorable vessel remodeling, suggesting that appropriate procedural strategies were critical for achieving effective results. The researchers noted that procedural factors played a vital role in ensuring that DCB treatment parallels the success rates of established interventions like drug-eluting stents (DES).
The study revealed that overall, 78% of the patients presented with acute coronary syndrome, and a median follow-up showed a low incidence rate of target lesion failure (5.2%). This retrospective analysis highlights that while DCB treatments have been recognized for their efficacy in treating in-stent restenosis, further examinations are required to refine their application to de novo lesions, where strategies have remained somewhat uncertain.
This understanding is further substantiated by examining how procedural complexities, including lesion preparation and balloon sizing techniques, directly dictated clinical outcomes. Also, by using intravascular ultrasound (IVUS) guidance, the study observed enhanced balloon sizing, leading to optimal treatment strategies.
Importantly, the implications of these findings suggest a need to reevaluate previously established clinical guidelines that assume a standard B-A ratio of around 0.8 to 1.0. Instead, this research elevates the conversation around employing larger ratios during DCB procedures to improve patient outcomes and refine existing practices within cardiac intervention.
Through these rigorous evaluations, the study adeptly illustrates that innovative adjustments to procedural frameworks can resonate positively in clinical practices. While substantial progress has been made, the authors advocate for additional trials to optimize the use of DCB treatment in CAD comprehensively.
In light of these results, it is evident that the future of DCB efficacy lies in the meticulous enhancement of procedural approaches. The dedication to refining these techniques holds promise not only for improving patient prognoses but also for shaping practice standards across cardiac intervention fields.
As the medical community continues to explore the best methods for employing DCB therapies, the insights gained from this study will be critical in promoting effective cardiovascular treatments and improving overall patient care.