Sepsis, typical for its severe immune reaction to infection, poses serious challenges for global health, with recent estimates placing incidence at about 48.9 million cases and 11 million deaths annually. Early diagnosis and effective treatment are key to improving survival rates, yet conventional methods are often inadequate, particularly concerning immune system suppression. The latest research has turned to genomic analysis and machine learning techniques to identify significant immune-related genes (IIRGs) associated with sepsis, aiming to create predictive models for diagnosis and treatment responses.
Conducted on two extensive genomic datasets, the study utilized methods such as the ESTIMATE algorithm, Weighted Gene Correlation Network Analysis (WGCNA), and various machine learning techniques to spot important immune genes. Eleven key IIRGs were identified, significantly correlated with known immune pathways and immune cell infiltration, offering valuable insights for both diagnosis and treatment protocols.
The study highlights the pressing need for innovations to address gaps in sepsis diagnosis, particularly concerning the immune response. Traditional markers like C-reactive protein and procalcitonin are often unreliable, making newfound strategies, like those using machine learning, increasingly important for improving patient care.
Machine learning models have shown promise, improving upon traditional methods with techniques such as Random Forest (RF) and eXtreme Gradient Boosting (XGBoost) to predict sepsis onset with increased accuracy. One proposed model, named SepsisFinder, claims to detect sepsis earlier and more effectively than conventional models. The integration of diverse machine learning approaches signals an important step forward for clinical applications, as these models offer high accuracy rates of over 75%.
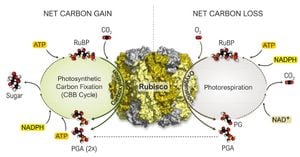
Key IIRGs identified through the study are primarily involved in significant immune signaling pathways. For example, pathways related to cytokine signaling play pivotal roles in regulating inflammation during sepsis. Understanding how these genes interact can illuminate the mechanisms governing patient responses to infection, potentially guiding therapeutic strategies.
A detailed analysis of immune infiltration has shown how specific IIRGs correlate with different immune cell levels present during sepsis. The correlation between GRB2, IL21R, and NCR3 with immune responses raises potential therapeutic directions. Future research ought to focus on validating these results and exploring these genes as biomarkers for personalized medicine.
Despite limitations such as sample bias and the need for clinical testing of predictive models, this study illuminates the path toward innovative and personalized approaches to tackling sepsis. Collaborative efforts across disciplines to deepen the knowledge of IIRGs, immune checkpoints, and their roles will be pivotal for paving new highways to effective clinical management of sepsis. The urgency for such strides is underscored not just by statistics but the fundamental need to improve sepsis outcomes globally.