A significant study has shown alarming links between C-reactive protein (CRP) levels, blood pressure (BP), and mortality risk among diabetic patients, underscoring the urgent need for monitoring these factors closely.
Data from the China Health and Retirement Longitudinal Study (CHARLS) revealed concerning findings about the growing threat posed by diabetes. With the prevalence of type 2 diabetes on the rise globally, particularly affecting Chinese adults, the study aimed to explore the effects of CRP and hypertension on the risk of all-cause mortality among patients suffering from this condition.
According to the analysis by researchers led by Jiamin Yan and Minzhe Zhang, the study sample consisted of 1,631 diabetic patients, averaging 60.7 years old, followed over seven years from 2011 to 2018. Alarmingly, 212 participants, equivalent to 13% of the cohort, died during this period. The authors wrote, "High CRP and hypertension were independently associated with increased risks for all-cause mortality among participants."
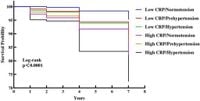
Through comparative analysis, several group classifications were established based on CRP and BP status, from low CRP/normotension to high CRP/hypertension. The results highlighted a stark reality: participants with high CRP levels and hypertension were at markedly higher risk for mortality, with the highest rates observed among the high CRP/hypertension group, reflecting their vulnerable health status.
During the study, the hazard ratios (HR) for different groups when compared to those with low CRP and normotension displayed troubling trends. High CRP levels resulted in HRs of 1.94 (95% CI 1.45–2.61) for all-cause mortality, with hypertension leading to HRs of 2.01 (95% CI 1.31–3.08). The combination of these two factors even more dramatically escalated risks. The authors emphasized, "The combination of high CRP and high BP significantly increased the risk of all-cause mortality in Chinese diabetic patients."
The background surrounding diabetes prevalence is sobering; as of 2021, more than 800,000 adults aged 20–79 years succumbed to diabetes-related complications, according to the latest statistics. This increase necessitates effective identification and management strategies to combat high levels of CRP and BP, significantly contributing to mortality rates.
Understanding these risk factors is pivotal, as previous research has suggested conflicting evidence concerning the role of CRP as a mortality predictor, particularly within diabetic populations. The current findings contribute to the conversation, highlighting how elevated CRP levels signify heightened inflammation and stress within the body, exacerbated by the strain of diabetes.
Methodologically, the CHARLS utilized rigorous sampling, encompassing various demographics across China. The study yielded insights not traditionally explored in such depth, especially with the significant cohort size. Prior studies primarily focused on individual factors when evaluating mortality risk, failing to address their combinatory impact.
During their analysis, researchers employed the Cox proportional hazard regression model to accurately assess the interplay between CRP, BP levels, and mortality, ensuring adjustments for additional confounding variables such as age, gender, education, marital status, and lifestyle factors, such as smoking and alcohol consumption.
The group dynamics within the research painted stark contrasts. For example, men and younger patients under 60 were observed to have elevated mortality risks when presenting with high CRP and BP, indicating underlying health disparities necessitating targeted attention.
Conclusions drawn from this study reveal the indispensable need for proactive healthcare measures aimed at reducing these biomarkers among diabetes patients. Monitoring CRP and BP could prove instrumental not only for improving the quality of life but also for extending longevity among patients with type 2 diabetes, which continues to be viewed as one of the foremost public health concerns.
Future studies may benefit from examining the variations of CRP and BP over time to see how changes might relate to shifts in mortality risk, as this aspect warrants focused exploration. Although contributing significantly to current science, the authors acknowledge potential limitations, including the inability to assess cause-specific mortality due to lack of data on specific death causes available within the CHARLS framework.
Despite these challenges, the research stands as a significant contribution to the field, providing prospective insights confirming the strong correlation between inflammatory markers and blood health indicators within diabetic populations.