As pulmonary infections continue to be a leading cause of hospitalization worldwide, recent research has highlighted innovative diagnostic methods that may transform patient care. A retrospective analysis conducted at Shenzhen Longgang Central Hospital showcases how metagenomic next-generation sequencing (mNGS) significantly enhances the identification of pathogens responsible for such infections. The study found that mNGS detected pathogens in 63.9% of patients, compared to just 27.8% identified through conventional microbiologic tests (CMT).
With the increasing incidence of pneumonia particularly affecting Chinese adults aged 60 and older, accurately diagnosing the diverse range of pathogens is a pressing need within the medical community. Previous studies have indicated that a substantial number of community-acquired pneumonia cases remain without any etiological diagnosis, posing challenges in clinical management. As the authors wrote, "mNGS serves as a valuable diagnostic approach for pulmonary infections, enhancing etiologic precision and informing patient management."
Implementing mNGS into the clinical workflow has made strides since its integration as a first-line diagnostic tool for urgent pathogen identification in 2021. The recent study analyzed 97 patients with suspected pulmonary infections who underwent mNGS alongside CMT over three years, showcasing mNGS's potential to outperform traditional methods.
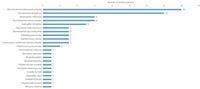
During the analysis, 75 distinct pathogen strains were identified among 63 patients, with notable findings including that Mycobacterium tuberculosis and Pseudomonas aeruginosa were among the most frequently detected pathogens. Over 77% of patients with positive mNGS results had their antibiotic regimens adjusted in response to the results, underscoring the clinical implications of accurate pathogen identification. The resulting clinical improvement was observed in 93.5% of these patients, demonstrating a significant benefit of mNGS in real-world settings.
Despite its advantages, the study did highlight challenges associated with mNGS, particularly the classification of microorganisms. Of the 138 potential strains initially identified by mNGS, a significant portion—47.1%—were later reclassified as colonizing organisms by physicians, raising important considerations about distinguishing between infection and colonization. This complexity calls for thorough clinical evaluation to accurately determine the clinical relevance of detected organisms.
Furthermore, the study's findings reflect broader implications. As existing pathogens like Mycobacterium tuberculosis remain a major concern in regions with high incidences, including China, improving methods for diagnosis through mNGS not only aids in treatment decisions but also may enhance public health efforts in addressing infectious diseases.
In conclusion, the integration of mNGS as a diagnostic tool in clinical practice shows considerable promise for managing pulmonary infections more effectively. Its ability to identify a wider spectrum of pathogens can aid healthcare providers in tailoring antibiotic therapies more accurately, ensuring better patient outcomes. As antibiotic resistance remains a global health concern, the insights gained from mNGS could lead to future advancements in infectious disease management.
However, the road ahead necessitates further research and prospective clinical trials to standardize the interpretative frameworks necessary for mNGS results. As technology continues to advance, so too does the potential for enhanced diagnostic capabilities in dealing with complex infections, paving the way for improved healthcare strategies going forward.