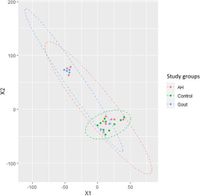
A recent study has unveiled significant insights into the relationship between gut microbiota and the metabolic disorders of hyperuricemia and gout. Researchers conducted a comprehensive analysis of the RNA from fecal samples taken from individuals with varying conditions, including healthy normouricemic controls, those with asymptomatic hyperuricemia (AH), and patients with gout. The study's findings reveal distinct gene expression patterns in the gut microbiome that correlate with these conditions.
In this groundbreaking research, the team evaluated samples from 26 individuals—10 healthy controls, 10 with AH, and six gout patients. They discovered that both AH individuals and gout patients exhibited an over-expression of Kyoto Encyclopedia of Genes and Genomes (KEGG) orthologues (KOs) primarily related to metabolic pathways such as pyruvate metabolism, purine metabolism, and the pentose pathway. Notably, the data indicated a striking log2 fold change for these pathways, reaching as high as Log2foldchange > 24 in the pentose pathway, with statistically significant p-values affirming these results (p-adj < 1.10 × 10−12).
The findings further revealed a marked decrease in expression for specific KOs associated with glycine metabolism in AH subjects, suggesting a complex interplay of microbial activity and urate homeostasis. For instance, the expression log2 fold change of KO related to glycine metabolism was noted at -18, compared to controls (p-adj < 1.72 × 10−6). In contrast, gout patients demonstrated a significant under-expression (Log2foldchange=-22.42, p-adj < 3.31 × 10−16) of KOs linked to phenylalanine biosynthesis.
Researchers have long examined how human gut microbiota relate to various metabolic dysfunctions, specifically hyperuricemia, which can lead to gout—a painful form of arthritis characterized by the accumulation of uric acid crystals in joints. Prior studies indicated that hyperuricemia is associated with various health issues, including type 2 diabetes and metabolic syndrome. Current data suggested that while many individuals experience hyperuricemia, only a fraction go on to develop gout. This highlights the clinical challenge of determining when to initiate treatment for AH subjects, which remains a point of contention in the medical community.
The research underscores a compelling hypothesis: gut bacteria influence the metabolism of purines, amino acids, and other compounds that directly impact urate levels. Using samples collected and analyzed from a controlled study, the researchers employed advanced bioinformatics techniques to map the various gene expressions against established metabolic pathways. The unique gut microbiota profile may lend insight into both the potential metabolic effects of probiotics and modulation therapies in managing urate levels effectively.
Significantly, the study’s differentially expressed KOs can serve as potential biomarkers for distinguishing between gout patients and those who are merely hyperuricemic. In their analysis, the authors emphasized that variations in gene expression within these pathways underscore the role that gut microbiota play not just in the development but perhaps in the prevention of advancing gout. The identified KOs include those involved in pyruvate metabolism—critical for generating energy and influencing inflammatory processes in the body.
Further validation of the study's findings demonstrated a clear association between specific KOs and the diagnosis of gout. For instance, the expression levels of K00161 and K00162 exhibited significant associations with a high odds ratio, highlighting the accuracy of these microbial signatures in predicting gout cases. Notably, the Receiver Operating Characteristic (ROC) curve analysis revealed an area under the curve (AUC) of 0.78 for K00161, with increased predictive accuracy when combinations of KOs were considered collectively.
This insightful research contributes to a growing understanding of the complex relationship between gut microbiota and metabolic disorders. The identification of a distinct gene expression pattern across different patient groups emphasizes the metabolic pathways influenced by microbiota, particularly concerning acetate production. Acetate is known to play a role in inflammatory responses, raising the possibility of dietary interventions capable of restoring balance in gut microbiota as a therapeutic approach to prevent gout flares.
However, the study does come with caveats, as all gout patients were under hypouricemic treatment at the time of analysis. This treatment may have influenced the microbiome's composition and functionality. Furthermore, the sample size was relatively small, which may limit the statistical power to detect weaker effects among various KOs.
The implications of this research are far-reaching, suggesting that modifying gut microbiota could potentially serve as a new avenue for managing gout and hyperuricemia. While the observed changes indicate an adaptive response to disease states, confirming the causal relationships between gut microbiota and gout will require longitudinal studies and further validation of metabolic pathways.
Moving forward, the researchers advocate for developing targeted probiotics that modulate these specific pathways, thereby reducing urate levels and preventing the recurrence of gout attacks. Overall, this pioneering study shines a light on the unique interplay between gut microbiota and metabolic disorders and emphasizes the need for continued research in this critical area of health.