Researchers are raising alarms over the declining efficacy of dihydroartemisinin-piperaquine (DHA-PPQ), a drug regarded for its role in the treatment and prevention of malaria, particularly in Africa. This study reveals that the protective effects of DHA-PPQ may weaken significantly against reinfection from Plasmodium falciparum, raising concerns for its widespread use.
In recent years, malaria has continued to impose a staggering burden, particularly in Africa where Plasmodium falciparum infections accounted for 96% of an estimated 263 million cases worldwide in 2023. The disease claimed over 597,000 lives, predominantly among children younger than five years. Countries across the African continent have turned to DHA-PPQ, noted for piperaquine’s long half-life that can suppress rapid reinfections.
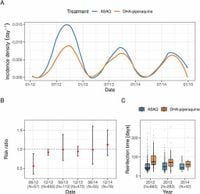
However, ongoing investigations indicate that the anticipated protective effects of DHA-PPQ might not hold under increased pressure from Plasmodium falciparum infections. A recent retrospective analysis examined clinical trial data involving 449 patients who received either DHA-PPQ or the older treatment artemisinin-amodiaquine for recurrent malaria episodes over two years. The study found that the risk of reinfection in patients treated with DHA-PPQ increased after the first season as plasmepsin gene copy number variations in the parasites became more prevalent.
The results indicated a higher frequency of reinfections among those treated with DHA-PPQ compared to those treated with artemisinin-amodiaquine during the follow-up period. The researchers noted, "the decline in post-treatment protection of DHA-PPQ upon repeated use in a high transmission setting raises concerns for its wider use for chemopreventive strategies in Africa."
Initial analyses of the data showed that while DHA-PPQ exhibited lower annual incidences of malaria compared to artemisinin-amodiaquine in the initial phases, this advantage diminished relatively quickly over time. The risk of reinfections for the DHA-PPQ group saw a notable rise, with risk ratios increasing from 0.58 after the first six months to nearly 1 by the end of the first year.
Interestingly, as DHA-PPQ was re-administered to patients, a trend of increasing plasmepsin 3 (pfpm3) multi-copy variants emerged, closely associated with piperaquine resistance. This genetic adaptation not only marked a shift in the infections observed but pointed to the pressing challenge of managing such resistance in high-transmission regions. The study reported a pull towards infections enriched in pfpm3 variations, suggesting a biological fitness advantage that allows these parasites to thrive even under drug pressure.
The findings compel experts to reconsider the sustainability of DHA-PPQ as a frontline treatment in malaria control. While the overall effectiveness of DHA-PPQ remains high throughout the study's duration, the implications of rising resistance markers cannot be ignored. Drug resistance could jeopardize efforts to contain the malaria burden, especially in settings experiencing intense transmission and frequent reinfections.
The authors assert that continued surveillance of pfpm copy number variations could serve as a valuable strategy for assessing the risk of impending drug resistance in African malaria populations. As they concluded, "the impact of plasmepsin mutations on large-scale preventive interventions needs to be considered.", highlighting the need for tailored resistance management strategies in the context of malarial epidemics.
This research underscores the delicate balance between utilizing effective treatments and the adaptive potential of malaria parasites, which may outpace current intervention methods unless proactive measures are employed. As countries in Africa look to enhance their malaria response strategies, understanding the genetic makeup of the infecting organisms, alongside treatment effectiveness, will be paramount.
Given the challenges and dynamics highlighted in this study, it becomes increasingly vital for researchers and public health officials to closely monitor drug effectiveness and resistance trends to shepherd effective malaria control efforts into the future.