A recent meta-analysis published in Scientific Reports on March 18, 2025, sheds light on the impact of various surgical techniques on pregnancy rates among women suffering from deep infiltrating rectal endometriosis. This study is significant as it aims to clarify confusion that has lingered around surgical options for a condition affecting reproductive health.
Endometriosis, a prevalent disorder impacting approximately 5-10% of women during their reproductive years, can lead to fertility challenges, particularly in cases of deep infiltrating endometriosis (DIE). The presence of DIE in the pelvic region disrupts normal anatomy, which can negatively influence the transport of gametes, along with implantation chances and raise miscarriage risks. Moreover, women with minimal endometriosis have shown lower fertility outcomes when comparing their experiences to healthy counterparts.
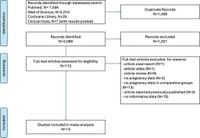
The aim of the meta-analysis was to analyze the effectiveness of colorectal resection in comparison to other surgical techniques such as rectal shaving and disc excision specifically regarding pregnancy outcomes. Researchers scrutinized studies published across various databases like PubMed, Cochrane Library, and more, identifying 13 studies that met the stringent eligibility criteria, collectively representing 3,248 patients. Pregnancy data were accessible from 2,131 of these patients, with diverse arrays of surgery documented.
Results from the analysis revealed that colorectal resection was associated with a lower pregnancy rate compared to the other surgical approaches. Specifically, the probability of pregnancy following colorectal resection was quantified at 35.5%, compared to 42.6% for other methods. Translated into statistical terms, colorectal resection showed an odds ratio (OR) of 0.64, indicating significantly lower chances of pregnancy in women undergoing this procedure (p < 0.001).
The findings further delineated outcomes when comparing colorectal resection directly against rectal shaving, illustrating that the less invasive procedure had dramatic advantages. The odds ratio for colorectal resection versus rectal shaving was noted at 0.51, marking a p-value of less than 0.001, signifying strong statistical significance in favor of rectal shaving.
However, when examining disc excision against colorectal resection, the metrics revealed that there was no substantial statistical difference. Here, the OR was figure at 0.65, indicating that while colorectal resection may not significantly undermine the chances for pregnancy in comparison to disc excision, the noted variability shows a need for further investigation.
In their conclusion, the authors emphasized the implications of these findings on the decision-making process for surgical interventions related to endometriosis. Since colorectal resection involves more extensive manipulation of pelvic anatomy, it could potentially lead to complications like postoperative adhesions that negatively influence fertility — a critical consideration when counseling patients about their surgical options.
intervention timelines and the nature of individual cases are paramount in determining suitable surgical techniques for complex endometriosis cases. The necessity of customizing treatment plans for patients, based on their unique situations, highlights the importance of shared decision-making in the clinical setting.
Although the findings are compelling, they are not without limitations. The authors noted considerable variability across the studies examined, with some not fully defining the surgical techniques used. Additionally, there were concerns about the potential biases among studies involved, which could influence outcomes and interpretations.
This research underscores the necessity for continued exploration, especially randomized controlled trials. Such studies should be aimed at clarifying the operational effectiveness of different surgeries concerning reproductive health and establish standardized criteria for reporting outcomes.
The growing awareness of the necessity for tailored surgical approaches will be critical moving forward. As the medical community strives to refine treatment protocols, patients can be better informed, leading to improved healthcare decisions that align more closely with their reproductive goals.