Headaches are notably common among patients with multiple sclerosis (MS), yet the underlying reasons for this association have remained elusive. A recent study from the Friedrich-Alexander University Erlangen-Nuremberg sheds light on the relationship between headaches and specific cerebral lesions in MS patients, suggesting that, for some, headaches may stem from lesions in areas of the brain responsible for pain processing.
Conducted between 2017 and 2023, researchers evaluated 48 MS patients suffering from headaches, alongside a control group of 92 MS patients without headaches, to ascertain the connection between headache occurrences and brain lesions. The study, published on March 23, 2025, reveals that most headache sufferers were females, with a significant mean age difference between the two groups: 51 ± 11 years for headache patients compared to 42 ± 11 years for those without.
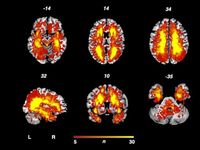
Utilizing voxel-based lesion symptom mapping (VLSM), the researchers correlated the presence of headaches with specific lesion clusters found in the left insula, left hippocampus, and right thalamus. These brain regions are known to play pivotal roles in processing pain, thereby offering an explanation as to why some MS patients experience persistent headaches.
Previous studies have suggested that headaches in MS may either be coincidental or develop as an underlying symptom of the disease itself. Recent findings indicate that neuroinflammation might facilitate headache onset during inflammatory MS activity. This reinforces the notion that headaches could potentially arise due to disruptions in pain processing pathways caused by cerebral lesions.
For instance, the thalamus influences pain signals that are relayed to the insula and periaqueductal gray matter, both essential to the brain's processing of pain. The presence of lesions at these sites can lead to abnormal pain sensations, a finding echoed by this study. Notably, lesions in the left insula have been associated with changes in how pain is perceived and processed emotionally, which could underpin headaches in MS patients.
Moreover, the hippocampus, another pivotal area identified in this research, is intricately linked to pain modulation—suggesting that lesions here may further contribute to heightened vulnerability to headaches.
The study's findings not only elucidate the complex interplay between MS lesions and headache development but also emphasize the need for further research into the implications of these results for clinical practice. With an increase in understanding of how headaches may be secondary to central nervous system lesions, medical professionals can better tailor their treatment strategies for MS patients.
The research team underscores that while specific brain lesions demonstrate an association with headache development, determining the nature of this relationship—in terms of whether headaches are primary or secondary—remains a challenging yet critical pursuit. They express hope that future studies will expand on these findings, further clarifying the interaction between MS pathophysiology and headache syndromes.
In conclusion, this recent study represents a significant step in contextualizing the often-overlooked relationship between headaches and MS. By identifying cranial lesions related to headache syndromes, the authors provide a foundation for improved comprehension of the disorder's complexity, paving the way for enhanced patient care and management strategies in those grappling with this debilitating disease.