In a recent study published in Nature, researchers investigated the in vitro antimicrobial activity of cephamycins and novel β-lactam/β-lactamase inhibitor combinations against extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli and Klebsiella pneumoniae isolates. The research found that more than 80% of these bacterial isolates displayed susceptibility to crucial antibiotics such as cefoxitin, cefmetazole, and flomoxef. This study highlights the ongoing struggle against antibiotic resistance, particularly as the prevalence of ESBL-producing organisms continues to rise in various clinical settings.
During the study, blood isolates were collected from three hospitals in Korea between January and May 2023. The urgency of finding effective treatments against these resistant bacteria cannot be overstated, as they pose significant health risks to patients. As reliance on carbapenems increases, so too does the need for effective alternatives to combat these infections.
One of the notable findings of this study was the effectiveness of cephamycins, a subgroup of second-generation cephalosporins. The study revealed that more than 80% of the ESBL-producing isolates were susceptible to a range of antibiotics, with impressive efficacy especially for combinations such as ceftazidime/avibactam and cefepime/enmetazobactam.
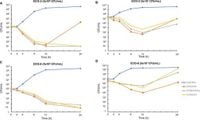
Particular attention was given to the inoculum effect, where the presence of a high bacterial load can significantly influence the efficacy of antibiotics. In this study, it was revealed that while cefoxitin, cefmetazole, and flomoxef maintained their effectiveness against standard inoculum sizes, their efficacy diminished notably at higher inoculum sizes. This led researchers to identify a worrying regrowth pattern following treatment with cephamycin after 12 hours.
The broader implications of this research are critical; with over 80% of the isolates showing susceptibility to certain treatments, it emphasizes the potential role of cephamycins as viable alternatives to carbapenem therapy. However, with substantial evidence pointing to reduced efficacy at high inoculum sizes, the clinical application of these antibiotics raises important questions regarding their deployment in emergency situations.
Furthermore, the study reinforces the necessity for ongoing surveillance and clinical trials to ensure that new treatments are thoroughly vetted. Understanding the implications of bacterial load on treatment success could shape protocols for managing severe infections and influence healthcare policies aimed at antibiotic stewardship.
In summary, cephamycins demonstrate promising potential to combat ESBL-producing bacteria according to their in vitro activity. Despite these findings, researchers urge caution due to signs of regrowth and diminishing efficacy at higher bacterial loads. As antibiotic resistance continues to be a global challenge, studies such as this underlie the importance of revisiting older antibiotics and systematically evaluating their effectiveness in contemporary scenarios.