Recent research has highlighted the complex migration patterns of human Th17 cells, particularly their dual roles involving transendothelial migration (TEM) associated with inflammation and arrest on activated endothelial cells (ECs). This study sheds light on the different roles played by chemokine receptors, particularly CCR2 and CCR6, which operate through unique mechanisms at each stage of T cell movement across vascular barriers.
Th17 cells, characterized by their ability to produce inflammatory cytokines like IL-17, are integral in both immunity and certain autoimmune diseases. Researchers have identified the markers and receptors necessary for these cells to migrate and enter inflamed tissues, leading to discoveries pertinent to diseases such as multiple sclerosis. The core finding indicates the distinction between arrest and migration processes concerning the positioning of chemokines.
The study determined the chemical environment where CCR2+ T cells exhibit pathogenic signatures, producing pro-inflammatory cytokines even without prior activation. Unlike CCR6 and CCR5, which mediate cell arrest on EC surfaces, CCR2 plays a pivotal role solely during TEM, warranting the need for its specific ligand concentration gradient for effective migration.
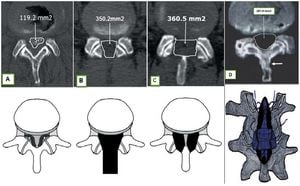
Investigations employed flow chamber assays using activated human umbilical vein endothelial cells (HUVECs) to simulate natural conditions of T cell migration. These assays clarified the sequential steps of rolling, arrest, and TEM, establishing how Th17 cells move efficiently through the endothelium during inflammatory responses. Only CCR6+(high)CCR2+ T cells successfully underwent TEM under these simulated conditions, showcasing the necessity of having distinct chemokine gradients.
This study also revealed the chemokine CCL20's localization on the surfaces of activated ECs, highlighting its role as integral to the cells’ arrest. Conversely, CCR2 ligands were largely absent from these surfaces, directing the focus on how these receptors need different chemokine environments to facilitate their respective roles. While research reveals the CCR2's incapacity for direct arrest, experiments displayed its importance for enabling TEM through orchestrated receptor activity and ligand availability.
The researchers examined various T cell subsets, identifying CCR6+(high)CCR2+ characteristics and pinpointing the pathological markers expressed during active inflammatory responses, always contrasting them against control groups. This process involved single-cell RNA sequencing, effectively mapping gene expression and providing detailed insight on how the CCR2+ cells' migratory abilities were linked to various phenotypic attributes.
Analysis of T cells from cerebrospinal fluid (CSF) of multiple sclerosis patients unveiled significant findings relating to the activation and pathogenic signatures of the CCR6+(high)CCR2+ subset. Such analysis is pivotal, as it reflects the changes these cells undergo when interacting with factors intrinsic to disease progression, thereby elucidifying pathways for potentially targeted therapies to mitigate inflammatory conditions.
All findings suggest specialized roles for chemokine receptors, with CCR2 uniquely facilitating T cell migration through gradients, distinct from arrest processes dictated by CCR5 and CCR6. This examination of the methodological framework can play a considerable role for future research focused on both the therapeutic targeting of these receptors and the broader comprehension of T cell dynamics, especially concerning autoimmune and inflammatory diseases.
With such discoveries, there is renewed interest and potential for developing novel strategies aimed at combatting the detrimental effects of these Th17 cells during autoimmune responses, contributing to therapeutic interventions targeting key pathways of T cell traffic.
Through purposeful identification of receptors linked to T cell extravasation and targeted intervention, it is possible to tailor therapies for conditions characterized by exaggerated inflammatory responses, thereby enhancing patient outcomes through precision medicine focused on T cell behavior.