British Columbia's healthcare system is undergoing significant scrutiny as recent changes, especially the restructuring of health ministries, come under the spotlight. Patients, healthcare advocates, and professionals—from cancer survivors to general practitioners—are voicing their concerns about delays and accessibility within the health services available to the public.
Earlier this year, the province initiated substantial reforms by merging several health ministries, including the absorption of the stand-alone mental health and addictions ministry. This shake-up is seen as aiming to streamline services amid challenges of rising wait times and emergency room closures, particularly affecting rural areas. The newly appointed health minister, Josie Osborne, acknowledges the gravity of these issues, pledging reform as her top priority. "Fixing emergency room closures is at the forefront of what I intend to achieve," Osborne announced, echoing the worries expressed by community members and physicians alike.
Concerns are mounting over the wait times for specialist consultations. Dr. Martin Daws, head of family practice at the University of British Columbia and himself a cancer survivor, pointed out the delays patients experience even before they are diagnosed. “It’s taking four or five weeks to see an oncologist for someone suspected of having cancer,” he said. This timeline is over twice as long compared to the national average, leaving patients scrambling for timely care.
Cancer advocacy groups like Cancer Action Now have taken the initiative to express their discontent through open letters to the new health minister. They argue the time taken to receive treatments and consultations is unacceptable. According to their findings, patients may wait nearly six weeks for treatment after their initial consultation, which places them at serious risk, especially when dealing with illnesses as time-sensitive as cancer.
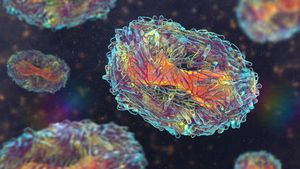
Beyond the waits, patients such as Phil Harbridge, who battled myeloma, recount harrowing experiences with the system. When Harbridge first exhibited concerning symptoms back in 2018, he attributed his fatigue to anemia, not realizing the severity of his condition until much later. His saga didn’t end with the diagnosis; he faced hurdles obtaining the necessary treatments approved for use. This included advocating for the use of Pomalidomide, which wasn't initially sanctioned for maintenance therapy within the province. Patients should not have to fight for treatment options, he remarked, emphasizing, “We need access now, not five years from now.”
These voices and stories are compelling readings for health policymakers and local authorities. Advocates underscored the need for immediate action to prune away the bureaucratic layers and enable faster access to care. The health ministry proudly states they have onboarded over seventy-one oncologists between April 2023 and March 2024, along with additional support staff, intending to make headway on treatment delivery. Still, critics say efforts must be more aggressive to keep up with the growing needs of the population.
Besides the extensive wait times for oncology services, the aftermath of recent restructuring has also revealed gaps within mental health services. The closure of the stand-alone mental health and addictions ministry has raised alarms among advocates who feel this move undermines the obliterated focus on mental health within the broader health agenda. Experts point out the precarious state of mental health services amid the opioid crisis and increasing mental illness rates exacerbated by the COVID-19 pandemic.
Over the years, British Columbia’s struggle with mental health and addiction has gained national attention. The urgent need for dedicated resources and specialized care has become apparent as many local communities continue to feel the negative impacts of substance abuse. The B.C. government’s decision to roll back on mental health ministries has left some wondering whether this will hinder progress toward improving services. Observers have labeled this restructuring as misguided, asserting the intention to streamline may only confuse and dilute care efforts.
Pledges to revitalize the mental health sector appear vague at best. Community organizations and mental health advocates argue the new structural changes contribute to fragmentation rather than unification, reducing clarity and responsiveness, especially during crises. Resources must target the uniquely intertwined issues of mental health, addictions, and medical care as they inform one another significantly.
Employing the clinical expertise of healthcare professionals is, of course, central to realizing efficient healthcare delivery. The correlation between mental wellness and physical health has long been established, wherein addressing one often alleviates issues within the other. Therefore, the administrative setups need to be adaptable and responsive to community needs rather than driven solely by the aim to consolidate bureaucracies.
The silent suffering of British Columbians grappling with wait times, closure of emergency services, and scarce support for mental health treatments portends challenges to public health. Advocacy groups insist the provinces must utilize community feedback and place patients at the center of health reforms if they wish to constructively move forward. The narrative must center on improving access, quality, and outcomes instead of merely adjusting administrative structures.
Nevertheless, hope remains. Previous successes, especially with expedited response efforts during health emergencies or increasing chronic illness management capacity, are mirrored with caution. Those within the system recognize the efforts of the health ministry but stress vigilance and accountability are required as programs roll out.
Citations of mismanagement from healthcare providers and advocates paint a detailed picture of the uphill battle health authorities face. Emphasis remains on prioritizing the accessibility of emergency services and how they directly impact patient outcomes. The recent advocacy struggles serve as reminders of the ultimate priority—the health and wellbeing of people across British Columbia—must inform all discussions and actions going forward.